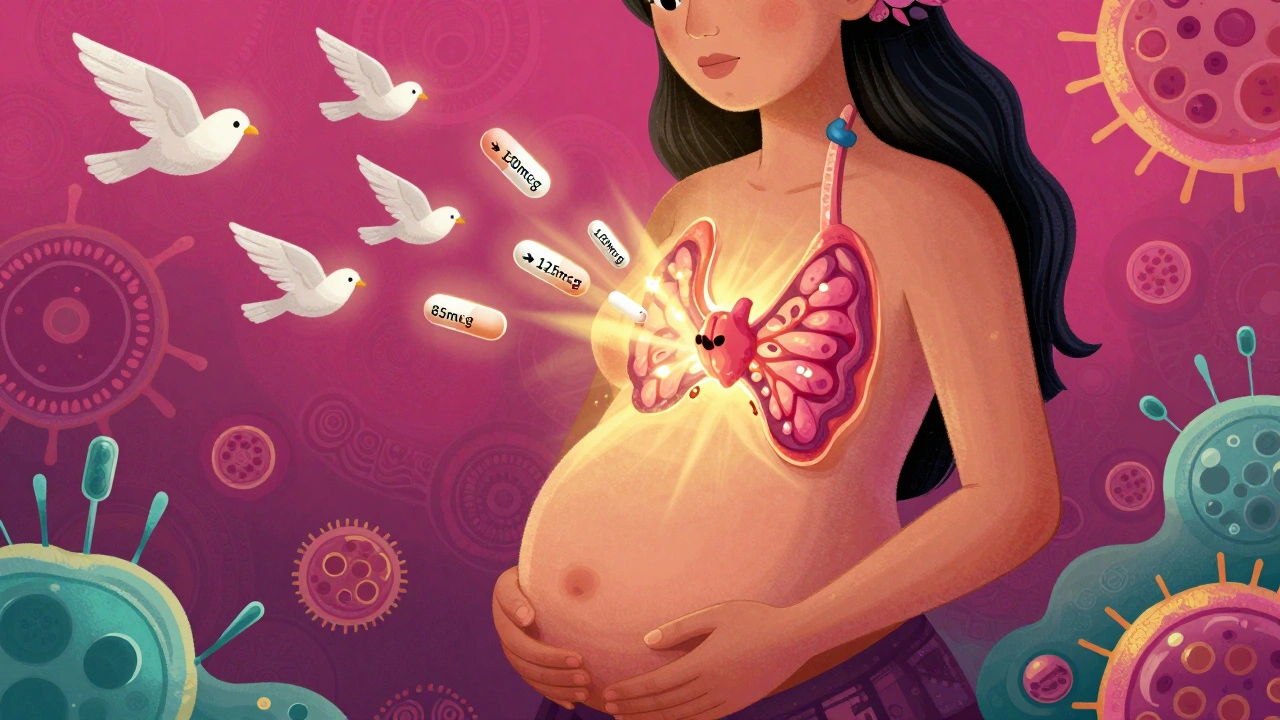
When you find out you're pregnant, your body starts changing in ways you can't always see. One of the most important but often overlooked changes is how your thyroid works. If you're already taking thyroid medication-usually levothyroxine-your dose isn't going to stay the same. In fact, most women need more medication almost immediately after conception. Skipping this adjustment can put your baby's brain development at risk.
Why Thyroid Medication Needs to Change During Pregnancy
Your thyroid gland makes hormones that control metabolism, energy, and, crucially, fetal brain development. Before 10 to 12 weeks, the baby can't make its own thyroid hormone. It relies entirely on what crosses the placenta from you. That’s why even a small drop in your thyroid hormone levels during the first trimester can affect your child’s IQ, attention, and learning abilities later in life. Studies show that women with untreated or poorly managed hypothyroidism during pregnancy have a 69% higher risk of miscarriage and a 23% higher chance of preterm birth. On the flip side, keeping your TSH in range can improve your baby’s cognitive scores by 7 to 10 points compared to untreated cases. That’s not a small difference-it’s the difference between needing extra help in school and thriving without it.How Much More Medication Do You Need?
Most women with pre-existing hypothyroidism need to increase their levothyroxine dose by 20% to 30% as soon as they confirm pregnancy. That might sound like a lot, but it’s not guesswork. Research from the National Institutes of Health found that women went from an average of 85.7 mcg per day before pregnancy to 100.0 mcg per day by the first trimester-an increase of nearly 15 mcg. That’s about one extra pill every few days. There are two common ways doctors handle this:- Take two extra doses per week (for example, take your pill on Monday and Thursday instead of just Monday).
- Or, if you're on a 100 mcg daily dose, increase it to 125 mcg right away.
- TSH ≥10 mIU/L: Start at 1.6 mcg per kg of body weight per day.
- TSH <10 mIU/L: Start at 1.0 mcg per kg per day.
What’s the Right TSH Target?
Not all guidelines agree on the exact TSH number you should aim for, but they all agree you need to stay below a certain threshold. The American Thyroid Association (ATA) recommends keeping TSH ≤2.5 mIU/L throughout pregnancy. The Endocrine Society says ≤2.5 in the first trimester and up to 3.0 in the second and third. Some experts, like Dr. Peter Laurberg, argue that pushing TSH too low might lead to overtreatment and unnecessary anxiety. But here’s the bottom line: if your TSH is above 2.5 in the first trimester, your risk of miscarriage goes up significantly. Real-world data backs this up. One study found that women with TSH over 2.5 in early pregnancy had a 69% higher miscarriage rate than those who stayed under it. And if you’re positive for thyroid antibodies (TPOAb), the Endocrine Society says you should aim even tighter-TSH under 2.5 the whole time.When and How Often Should You Get Tested?
Testing isn’t a one-time thing. You need to check your TSH frequently because your body’s demand keeps changing. Here’s what the experts recommend:- Test within 4 weeks of confirming pregnancy.
- Test every 4 weeks until your dose is stable.
- Then check again at 24-28 weeks and 32-34 weeks.
How to Take Your Medication Correctly
Taking your pill wrong can make all the difference. Levothyroxine is absorbed poorly if you take it with food, coffee, calcium, or iron. Follow these rules:- Take it on an empty stomach, first thing in the morning.
- Wait 30 to 60 minutes before eating or drinking anything besides water.
- Avoid calcium supplements, prenatal vitamins with iron, or antacids for at least 4 hours after taking your pill.
What About Breastfeeding?
Good news: levothyroxine is safe while breastfeeding. Only tiny amounts pass into breast milk, and studies show no effect on the baby’s thyroid function or development. You can keep your pregnancy dose or slightly reduce it after delivery-your doctor will guide you. Don’t stop or lower your dose on your own. Your thyroid needs time to reset after pregnancy, and stopping too soon can lead to postpartum hypothyroidism.
What’s New in 2025?
The field is moving fast. In 2023, the American Thyroid Association reversed its long-standing position and now recommends universal TSH screening for all pregnant women in the first trimester. That’s a big shift-from screening only high-risk women to testing everyone. New tools are helping too. The ENDO trial in 2022 used artificial intelligence to predict individual dose needs based on pre-pregnancy TSH, weight, and antibody status. Women using AI-guided dosing had 28% better TSH control than those on standard protocols. There’s also a mobile app called MyThyroid, used by over 12,500 pregnant women since 2019. Eighty-seven percent said it helped them stick to their schedule and reduce anxiety.What If You Can’t Get Care?
Globally, access to levothyroxine is still unequal. In low-income countries, only 22% have consistent access to the medication. That contributes to 15% of preventable developmental delays in children. The World Health Organization added levothyroxine to its Essential Medicines List for maternal health in 2023, signaling that this isn’t just a personal health issue-it’s a public health priority.What to Do Next
If you’re pregnant or planning to be:- Check your current TSH level before conception if possible.
- As soon as you get a positive test, contact your endocrinologist or doctor. Don’t wait for your first OB appointment.
- Ask for a TSH test within 4 weeks of confirmation.
- Take your levothyroxine correctly-on an empty stomach, away from supplements.
- Keep track of your doses and test dates. Use a calendar or app.
Can I stop taking thyroid medication during pregnancy?
No. Stopping thyroid medication during pregnancy can lead to serious complications, including miscarriage, preterm birth, and lower IQ in your child. Levothyroxine is safe and essential. Your dose may need to increase, but never stop without medical advice.
Will my thyroid medication affect my baby?
No. Levothyroxine is a synthetic form of the natural thyroid hormone your body makes. It crosses the placenta in tiny amounts, but studies show no harm to the baby. In fact, it’s critical for brain development. Untreated hypothyroidism is far more dangerous than the medication.
How soon after pregnancy should I adjust my dose back down?
After delivery, most women can return to their pre-pregnancy dose within 6 to 8 weeks. Your doctor will check your TSH around 6 weeks postpartum to confirm. Don’t reduce your dose on your own-your body is still adjusting hormonally.
Can I take levothyroxine with my prenatal vitamin?
No. Prenatal vitamins often contain iron and calcium, which block levothyroxine absorption. Take your thyroid pill at least 4 hours before or after your prenatal vitamin. Many women take their thyroid pill in the morning and the prenatal vitamin at lunch or dinner.
Is universal TSH screening really necessary?
Yes. The American Thyroid Association now recommends testing all pregnant women in the first trimester because up to half of women with hypothyroidism don’t know they have it. Symptoms like fatigue and weight gain are often mistaken for normal pregnancy changes. Screening catches cases early and prevents long-term harm to the child.
an mo
December 6, 2025 AT 06:10Let’s be real-this isn’t just about levothyroxine dosing, it’s about systemic neglect in maternal endocrinology. The 20-30% increase isn’t a suggestion, it’s a physiological imperative. TSH thresholds haven’t been updated since the Stone Age, and ACOG’s 50 mcg jump is still too conservative. We’re talking about neurodevelopmental trajectories here, not just lab values. If you’re waiting for a prenatal visit to adjust, you’re already behind. The placenta doesn’t care about your insurance pre-auth.
And don’t get me started on how Medicaid patients in rural states can’t even get TSH tests done before week 8. This isn’t medicine. It’s triage with a stethoscope.
aditya dixit
December 7, 2025 AT 01:25There’s a quiet wisdom in how the body knows before the mind does. Pregnancy doesn’t wait for appointments or lab reports. The thyroid, in its ancient rhythm, demands more the moment life begins to form. A 15 mcg increase isn’t arbitrary-it’s biological poetry. We treat it like a math problem, but it’s a covenant: your body gives, and in return, it asks only for a little more. Not greed. Not excess. Just enough to carry another soul into the world.
Let’s stop reducing this to dosage charts. It’s about honoring the invisible work of motherhood-hormonal, emotional, cellular.
Mark Ziegenbein
December 7, 2025 AT 07:34Look I’ve read every paper from the Endocrine Society to the Cochrane reviews and let me tell you the data is not just compelling-it’s revelatory. We’re not talking about marginal gains here we’re talking about a 7 to 10 point IQ differential which if you think about it in terms of standardized testing is the difference between being in the 75th percentile and the 30th percentile which means your kid might not get into the gifted program or worse might need IEP services and who wants that when all it takes is a simple pill adjustment
And don’t even get me started on how OBs still think TSH under 5 is fine during pregnancy no it’s not it’s 2.5 and even that’s borderline because the placental deiodinase enzymes are already ramping up by week 4 and if you’re not on 125 mcg by then you’re playing Russian roulette with your child’s frontal lobe development
Also why are we still using mcg and not mcg/kg body weight for new diagnoses this is 2025 not 1998
Juliet Morgan
December 7, 2025 AT 09:12i wish someone had told me this before i lost my first pregnancy. i was on 75mcg, got pregnant, didn't change anything, and by week 7 my tsh was 8.2. no one mentioned it until my second trimester. by then it was too late. i’m not mad, just heartbroken. if you’re reading this and you’re on levo-call your endo TODAY. don’t wait for the appointment. your baby’s brain is already listening.
Norene Fulwiler
December 8, 2025 AT 15:08My cousin in Lagos had to drive 3 hours to get her thyroid meds during pregnancy. No labs. No doctors. Just a pharmacy that sold levothyroxine without a script. She took what she could. Her son is 4 now-brilliant, talks in full sentences, loves math. If she could do it with no support, imagine what we could do with access.
This isn’t just a US problem. It’s a global silence.
Ada Maklagina
December 9, 2025 AT 14:28my doc upped me to 125 right away. felt weird at first. like my heart was racing. then i realized it was just my body catching up. no more brain fog. no more crying over spilled coffee. my husband said i smiled more. weird how a pill can change your whole vibe.
also i started taking it on an empty stomach. no coffee for 45 mins. game changer.
Harry Nguyen
December 11, 2025 AT 00:05Oh great another fearmongering article about how every pregnant woman is one missed pill away from having a child who can’t tie their shoes. Let me guess-next you’ll tell us caffeine causes autism and walking barefoot on grass gives babies ADHD
Meanwhile in Sweden they don’t even test TSH during pregnancy and their IQ scores are higher than ours. Maybe the real issue is our obsession with quantifying motherhood into lab values instead of trusting biology
Also 50 mcg increase immediately? That’s not medicine that’s a pharmaceutical marketing campaign
Laura Saye
December 12, 2025 AT 17:05What strikes me most isn’t the dosage numbers-it’s how little we talk about the emotional weight of this. You’re not just adjusting a pill. You’re adjusting your identity. One day you’re managing hypothyroidism like a chronic condition, the next you’re responsible for two lives. The anxiety of getting it ‘right’ is its own kind of exhaustion.
I kept a journal. Every time I took my pill, I wrote down how I felt. Some days I was calm. Some days I cried because I was terrified I’d mess it up. I didn’t know if I was doing enough. Maybe we need more than TSH targets. Maybe we need more space to say: I’m scared. I’m trying. I need help.
And if you’re a provider reading this-don’t just hand out a script. Ask how they’re sleeping. Ask if they’re afraid. The numbers matter. But so does the silence between them.