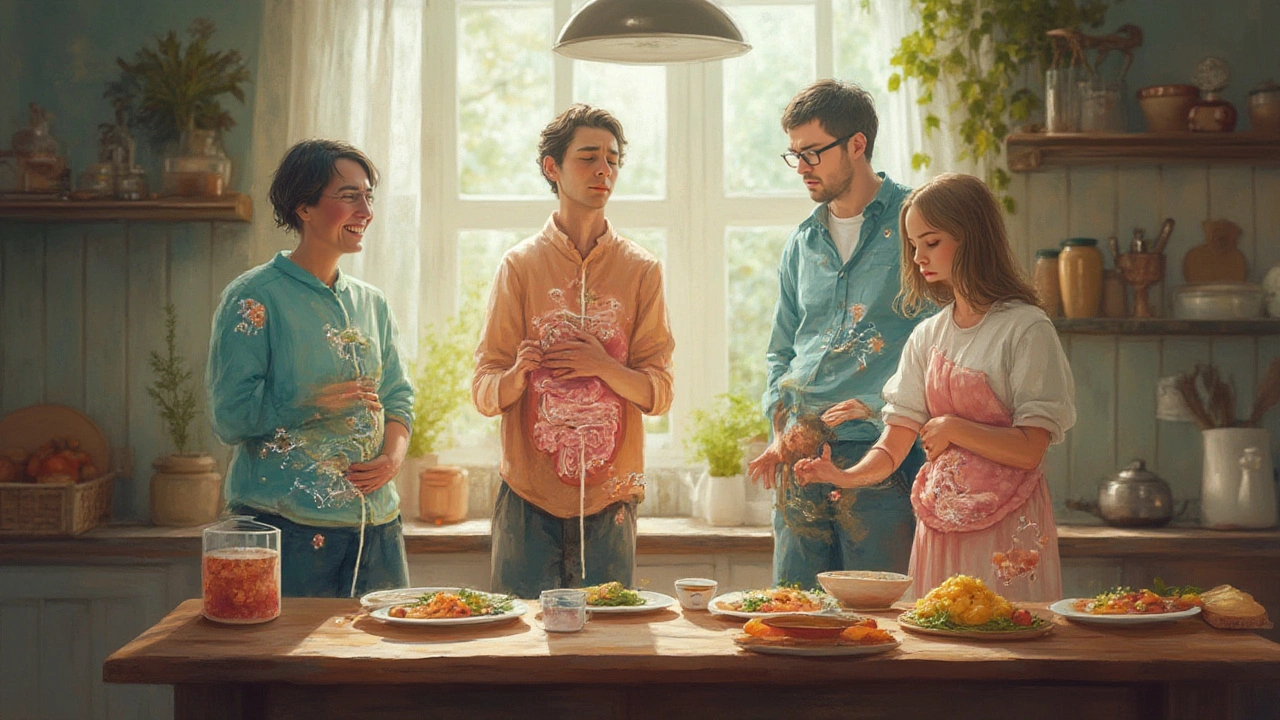
Intestinal Health: Simple Ways to Keep Your Gut Happy
Feeling bloated, dealing with frequent trips to the bathroom, or just not getting that "right" feeling after meals? Your gut is a busy organ that needs the right fuel, routine, and sometimes a little medical help. Below you’ll find easy habits to protect your intestinal health and know when it’s smart to reach for a medicine.
Everyday habits for a strong gut
First up, food. Aim for a mix of fiber‑rich veggies, whole grains, and fruits. Fiber adds bulk to stool and feeds good bacteria, which keep digestion smooth. If you’re not used to high‑fiber meals, add them gradually – sudden spikes can cause gas or cramping.
Water is the unsung hero. Staying hydrated helps fiber do its job and prevents hard stools that can turn a simple constipation episode into a painful ordeal. A good rule of thumb is eight glasses a day, but if you’re active or live in a hot climate, sip a bit more.
Mindful eating matters. Chew each bite thoroughly and avoid eating while scrolling on your phone. Slow eating gives your stomach time to signal fullness and reduces the chance of indigestion.
Stress isn’t just mental; it hits your gut too. Practicing brief breathing exercises, a short walk, or even a quick stretch after meals can calm the nervous system and keep gut muscles moving at a normal rhythm.
When meds become necessary
Even with the best habits, you might hit a snag. Acute diarrhea, for instance, can strike after a bad food bout or a viral infection. Over‑the‑counter loperamide (brand name Imodium) works by slowing gut movement, letting your body re‑absorb fluid and firm up stools. Use it as directed – usually no more than two doses in 24 hours – and stop if symptoms linger beyond two days without improvement.
For chronic issues like IBS‑D (irritable bowel syndrome with diarrhea), a doctor might suggest a low‑dose prescription of the same ingredient or a different agent that targets gut receptors. The key is to follow professional guidance and never self‑prescribe long‑term without a check‑up.
Some medications you take for other health problems can affect intestinal health too. Metformin, a common diabetes drug, often causes mild diarrhea in the first weeks. Staying hydrated, taking it with food, and timing the dose (usually with the evening meal) can lessen the upset.
If you suspect a medication is hurting your gut, talk to your pharmacist or doctor. They might switch you to an alternative or adjust the dose. Never stop a prescription abruptly without advice.
Probiotics are another tool that many people find helpful. Look for products containing proven strains like Lactobacillus rhamnosus GG or Bifidobacterium infantis. While not a cure‑all, they can restore balance after a course of antibiotics or a bout of food poisoning.
Finally, keep a simple symptom log. Note what you eat, how you feel, and any meds you take. Over time you’ll spot patterns that help you and your doctor fine‑tune a plan tailored to your gut.
Keeping intestinal health on track doesn’t have to be complicated. A mix of smart food choices, proper hydration, stress management, and informed use of medication can keep your digestion running smoothly. If you notice persistent changes, reach out to a healthcare professional – early action often prevents bigger problems down the road.
- Celeste Farnell
- 5-07-25
- Health & Medicine
How Enteric Infections Impact Gut Health: Risks, Symptoms, and Recovery
Unpack how enteric infections like stomach bugs disturb your gut health, which signs to watch out for, and science-backed ways to recover. Support your gut’s comeback.
Details