What Exactly Is a Stroke?
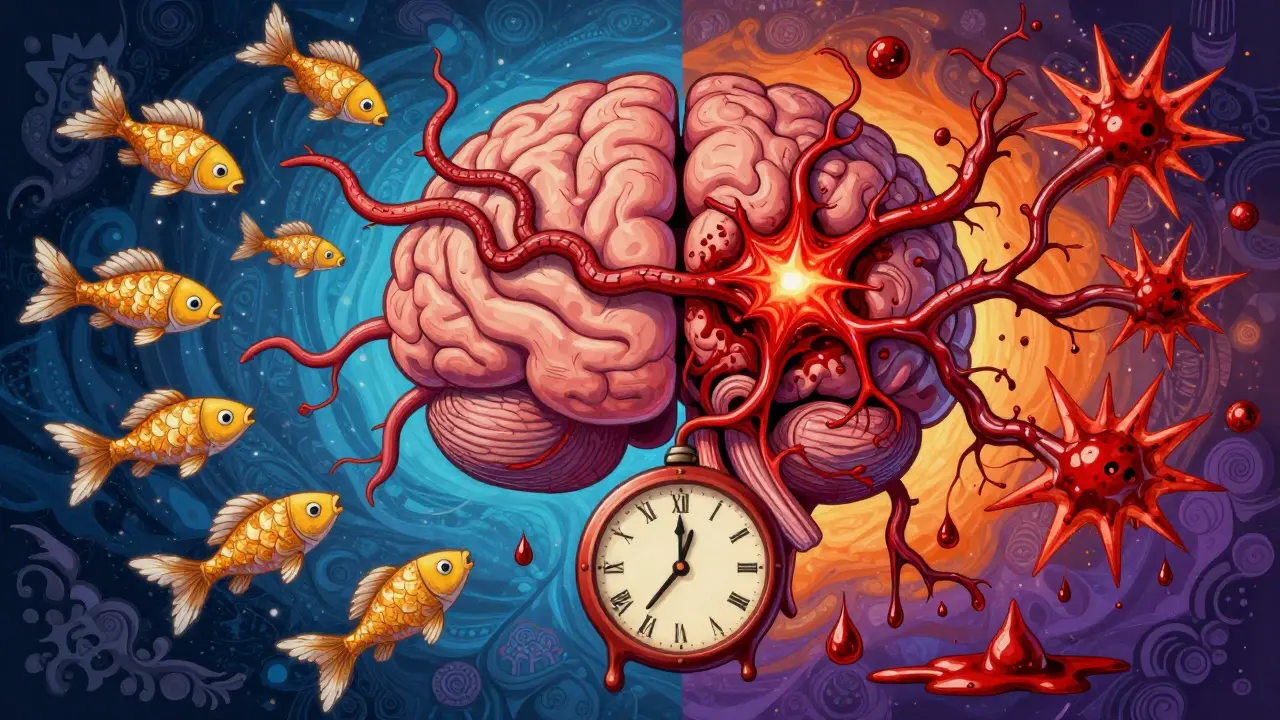
A stroke happens when the blood supply to part of your brain gets cut off or leaks. Without oxygen, brain cells start dying within minutes. That’s why every second counts. There are two main types: ischemic and hemorrhagic. Together, they make up nearly all strokes. Knowing the difference isn’t just academic-it can save your life or someone else’s.
Ischemic Stroke: The Blocked Artery
Ischemic strokes account for about 87% of all strokes. This happens when a blood clot blocks an artery leading to your brain. The clot might form right there in your brain (thrombotic), or it could travel from somewhere else-like your heart (embolic). About half of all ischemic strokes are thrombotic, often caused by fatty buildup in large arteries. The other big chunk, around 25%, are small vessel strokes, called lacunar strokes, which happen in tiny arteries deep inside the brain.
These strokes don’t always hit like a lightning bolt. Symptoms can creep in over minutes or even hours. Someone might wake up with numbness on one side, struggle to speak clearly, or feel dizzy. Sometimes, the warning signs are mild at first, which is why people delay calling 999. But don’t wait. Even if symptoms seem to fade, it could be a mini-stroke (TIA), a major red flag.
Hemorrhagic Stroke: The Ruptured Vessel
Hemorrhagic strokes are less common-only 13-15% of cases-but often more deadly. Instead of a blockage, a blood vessel bursts inside or around the brain. This causes bleeding, which presses on brain tissue and increases pressure. There are two kinds: intracerebral hemorrhage (bleeding inside the brain) and subarachnoid hemorrhage (bleeding on the surface, often from a ruptured aneurysm).
This type of stroke usually strikes suddenly. People describe it as the worst headache of their life-like being hit with a hammer. Other signs include vomiting, seizures, confusion, unequal pupils, or sudden loss of consciousness. High blood pressure is the #1 cause. Nearly 8 out of 10 intracerebral bleeds happen because decades of uncontrolled hypertension have weakened the vessel walls.
How Symptoms Differ Between Types
It’s not just about speed. The symptoms themselves can hint at the type. A 2017 study of over 500 stroke patients found that:
- 92% of hemorrhagic stroke patients had a severe headache-only 19% of ischemic patients did.
- Seizures happened in 17% of hemorrhagic cases, but almost never in ischemic ones.
- Agitation was seen in 80% of hemorrhagic cases, but just 7% of ischemic.
- Dilated or unequal pupils were common in hemorrhagic strokes, rare in ischemic.
These aren’t foolproof clues, but they help medics decide fast. If someone collapses with a thunderclap headache and seizures, hemorrhagic stroke is high on the list. If someone slowly loses speech and arm strength, ischemic is more likely.

How Doctors Diagnose Stroke Type
When someone arrives at the hospital with stroke symptoms, the first thing they do is get a CT scan. It’s quick, widely available, and shows whether there’s bleeding. If the scan is clear, they’ll likely do an MRI to look for clots. Time matters. The faster they know the type, the faster they can treat it.
Some hospitals now use AI tools like Viz.ai to flag stroke cases automatically. These systems can detect clots in brain scans within seconds, cutting down delays. In 2022, hospitals using this tech reduced the time to give clot-busting drugs by over 50 minutes.
Treatment: Clot Busters vs. Surgery
Treatment is completely different depending on the stroke type.
For ischemic strokes, doctors give clot-dissolving drugs like alteplase or tenecteplase. These work best if given within 4.5 hours of symptom start. For larger clots in major arteries, they can do a mechanical thrombectomy-using a device to physically pull the clot out. This can be done up to 24 hours after symptoms begin, if imaging shows there’s still salvageable brain tissue.
Hemorrhagic strokes don’t respond to clot-busters. In fact, giving them could make bleeding worse. Instead, treatment focuses on stopping the bleed and reducing pressure in the skull. This might mean surgery to clip an aneurysm, coil it from inside the artery, or drain blood with a minimally invasive procedure. Blood pressure control is critical-too high, and bleeding continues; too low, and the brain doesn’t get enough blood.
Preventing Ischemic Stroke
Most ischemic strokes are linked to heart and artery problems. The biggest risk? Atrial fibrillation (AFib)-an irregular heartbeat that lets blood pool and clot. People with AFib have a 500% higher stroke risk. The fix? Anticoagulants like apixaban or warfarin. The ARISTOTLE trial showed these drugs cut stroke risk by 60-70%.
For those without AFib, daily low-dose aspirin or clopidogrel reduces the chance of a second stroke by 25%. But these aren’t for everyone-talk to your doctor first.
Lifestyle changes make a huge difference. The Mediterranean diet (rich in olive oil, fish, nuts, vegetables) cut stroke risk by 30% in the PREDIMED study. Walking 150 minutes a week lowers your risk by 27%. Quitting smoking cuts your stroke risk in half within one year.
Preventing Hemorrhagic Stroke
This one’s simpler: control your blood pressure. It’s the #1 preventable cause. The SPRINT trial showed that keeping systolic pressure below 120 mmHg-instead of the old target of 140-reduced hemorrhagic stroke risk by 38% in high-risk people.
That doesn’t mean you need to be perfect. Even small, steady improvements help. Cutting salt, losing weight, exercising, and limiting alcohol all lower blood pressure. If you’re on medication, take it as prescribed. Skipping doses is a silent killer.
Also, avoid blood thinners unless you need them. If you’re on anticoagulants for AFib, your doctor will balance your stroke risk against bleeding risk. Never start or stop these meds without medical advice.
What You Can Do Right Now
You don’t need to wait for a diagnosis to act. Here’s what works:
- Know your blood pressure. Get it checked at least once a year. If it’s over 130/80, talk to your doctor.
- If you have AFib, don’t ignore it. Take your prescribed blood thinner.
- Quit smoking. Even one cigarette a day raises your risk.
- Move more. Walk, swim, dance-anything that gets your heart pumping.
- Eat real food. Cut processed snacks, sugar, and fried stuff. Focus on vegetables, beans, fish, and whole grains.
- Learn FAST: Face drooping, Arm weakness, Speech difficulty, Time to call 999. Don’t wait. Don’t drive yourself. Call emergency services immediately.
Why Timing Is Everything
Every minute a stroke goes untreated, 1.9 million brain cells die. That’s why the phrase “time is brain” isn’t just a slogan-it’s biology. The sooner you get help, the less damage you’ll have.
Studies show that patients who reach the hospital within 60 minutes of symptoms have a 40% better chance of full recovery. That’s why recognizing the signs fast matters more than knowing the exact type. Call 999 if you see any of these: sudden numbness, confusion, trouble speaking, vision loss, dizziness, or a terrible headache.
What’s New in Stroke Care
Research is moving fast. In 2023, the WAKE-UP trial showed that MRI can identify stroke patients who still have salvageable brain tissue up to 9 hours after symptoms start. That means more people might qualify for clot-busting drugs.
For hemorrhagic strokes, the MISTIE III trial found that a minimally invasive surgery using a tiny tube and clot-dissolving drug reduced death rates by 10% over a year.
And now, there’s a blood test that can tell ischemic from hemorrhagic stroke in under 15 minutes by measuring a protein called GFAP. It’s not in every hospital yet, but it could one day let paramedics start treatment before the patient even arrives.
Final Thought: Prevention Beats Cure
Stroke is still the fifth leading cause of death in the U.S. and a major cause of long-term disability. But here’s the good news: up to 80% of strokes are preventable. You don’t need fancy gadgets or expensive treatments. You need awareness, consistency, and action.
Control your blood pressure. Take your meds. Move daily. Eat well. Quit smoking. Know the signs. If you see them, call 999-no excuses.
Can you have a stroke and not know it?
Yes. Small vessel strokes, called silent strokes, can happen without obvious symptoms. They’re often found on brain scans done for other reasons. But even silent strokes damage brain tissue and increase your risk of a major stroke later. That’s why controlling blood pressure and checking for AFib matters-even if you feel fine.
Are strokes only a problem for older people?
No. While stroke risk increases with age, more than 1 in 4 strokes now happen in people under 65. Younger people are getting strokes due to rising rates of obesity, diabetes, high blood pressure, and smoking. Even teens and young adults can have strokes from heart conditions, blood disorders, or drug use. Don’t assume it can’t happen to you.
Can aspirin help during a stroke?
No. Don’t give aspirin during a stroke unless a doctor tells you to. If it’s a hemorrhagic stroke, aspirin can make bleeding worse. The only safe move is calling 999 immediately. Emergency responders will determine the right treatment on arrival.
What’s the difference between a TIA and a stroke?
A TIA (transient ischemic attack) is a mini-stroke. Symptoms are the same-numbness, speech trouble, vision loss-but they last less than an hour and don’t cause permanent damage. But it’s not a warning you can ignore. Nearly 1 in 3 people who have a TIA will have a full stroke within a year. Treat it like an emergency. Get checked immediately.
Is recovery possible after a hemorrhagic stroke?
Yes, but it’s harder. Hemorrhagic strokes often cause more initial damage, and recovery takes longer. But with intensive rehab-physical therapy, speech therapy, occupational therapy-many people regain function. The key is early, consistent rehab and managing blood pressure to prevent another stroke. Some people make near-full recoveries; others need ongoing support. Progress is possible at any age.
Stroke isn’t a death sentence. It’s a call to act-before it happens, or the moment it does. Your brain doesn’t ask for permission. Neither should you.
Kunal Majumder
January 10, 2026 AT 01:38Saumya Roy Chaudhuri
January 10, 2026 AT 01:43Ted Conerly
January 11, 2026 AT 00:58Jaqueline santos bau
January 12, 2026 AT 01:35anthony martinez
January 13, 2026 AT 14:02Ian Cheung
January 15, 2026 AT 00:21Aurora Memo
January 16, 2026 AT 00:19Jay Amparo
January 16, 2026 AT 09:54chandra tan
January 16, 2026 AT 17:15Mario Bros
January 18, 2026 AT 06:16Faith Edwards
January 18, 2026 AT 15:36Lisa Cozad
January 19, 2026 AT 15:35Dwayne Dickson
January 21, 2026 AT 08:13