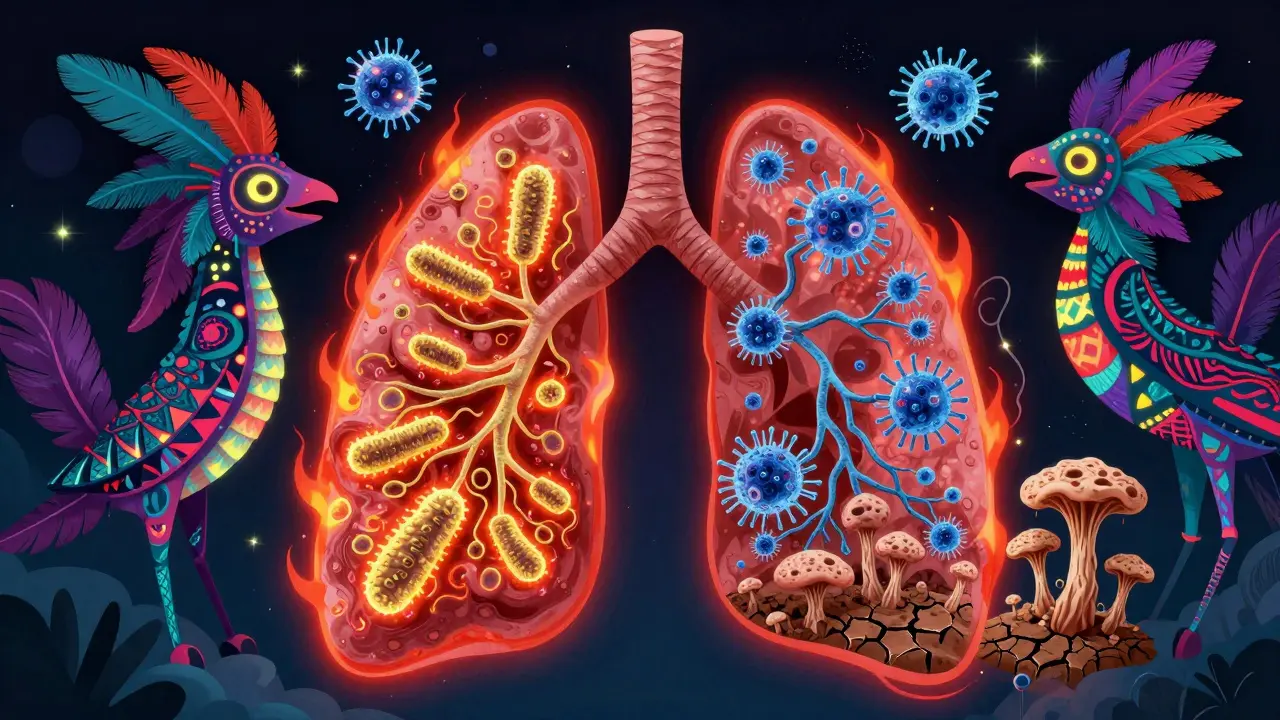
When you hear the word pneumonia, you might think of a bad cold that turns serious. But pneumonia isn’t one thing-it’s a group of infections that affect your lungs in very different ways. The kind of germ causing it changes everything: how you feel, how doctors treat it, and even how likely you are to recover. Knowing the difference between bacterial, viral, and fungal pneumonia isn’t just medical jargon-it can save your life.
Bacterial Pneumonia: The Sudden Onset
Bacterial pneumonia is the most common type, responsible for about half of all community cases. The biggest culprit? Streptococcus pneumoniae is a bacterium that causes over 12% of severe pneumonia cases in young children and remains the top cause worldwide. It doesn’t sneak up-it hits hard. One day you feel okay, the next you’re running a fever of 104°F, coughing up thick yellow or green mucus, and struggling to breathe. Your chest hurts when you take a deep breath. Your lips or fingernails might turn blue because your body isn’t getting enough oxygen.
Doctors can often spot it on a chest X-ray: a solid white patch in one lobe of the lung. That’s called lobar consolidation. It means the tiny air sacs (alveoli) are filled with fluid, pus, and dead cells. Your immune system responds with a flood of neutrophils-white blood cells that swarm the infection like firefighters. But if left untreated, this can turn deadly. About 5-7% of people hospitalized with bacterial pneumonia don’t survive.
Treatment is straightforward: antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin are usually the first line. For atypical bacteria like Mycoplasma pneumoniae is a bacterium causing "walking pneumonia," often milder but highly contagious in schools and workplaces., doctors use different drugs. The key? Start antibiotics early. Delaying them increases the risk of complications like sepsis or lung abscesses.
Viral Pneumonia: The Slow Burn
Viral pneumonia makes up about one-third of cases. Unlike bacterial pneumonia, it doesn’t always start in the lungs. It often begins as a runny nose, sore throat, or cough-like a regular cold. Over the next few days, it moves deeper. You feel tired, achy, and develop a dry cough that gets worse. Fever is usually lower-around 100-102°F-and comes on slowly.
The big players? Influenza A and B are viruses responsible for 20-30% of viral pneumonia cases during flu season., RSV (Respiratory Syncytial Virus) is a virus that causes severe pneumonia in infants and older adults., and SARS-CoV-2 is a virus that can cause pneumonia with bilateral lung involvement, especially in unvaccinated individuals.. These viruses don’t just attack your lungs-they trigger a wave of inflammation across both lungs. That’s why chest X-rays show a hazy, patchy pattern instead of one solid white area.
Antibiotics? Useless. You can’t kill a virus with them. Instead, treatment is supportive: rest, fluids, oxygen if needed. For flu, antivirals like oseltamivir (Tamiflu) can help if started within 48 hours. For severe COVID-19, remdesivir may be used. The real danger? Secondary infection. About 1 in 4 people with severe flu end up with bacterial pneumonia on top of it-usually from Staphylococcus aureus is a bacterium that can cause life-threatening pneumonia after viral illness. or Streptococcus pneumoniae is a bacterium that commonly causes secondary pneumonia after viral infection..

Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare in healthy people. But if your immune system is weak-because of HIV, cancer treatment, organ transplants, or long-term steroids-you’re at risk. It’s not something you catch from a sneeze. You breathe it in from the soil.
Coccidioides is a fungus causing Valley fever, endemic in the southwestern U.S., with 20,000 cases reported yearly. lives in dry, dusty soil in places like Arizona and California. Histoplasma capsulatum is a fungus found in bird and bat droppings, with 65% of people in the Ohio and Mississippi River valleys exposed without symptoms. hides in soil enriched with droppings. Blastomyces dermatitidis is a fungus causing blastomycosis, common in the Midwest and Great Lakes region, with 1-2 cases per 100,000 people annually. thrives in moist soil near rivers.
People who work outside-farmers, landscapers, construction workers-are at higher risk. You don’t get sick right away. Symptoms can take weeks to show: fever, cough with phlegm, night sweats, even weight loss. It can look like tuberculosis or bacterial pneumonia. That’s why diagnosis is tricky. Blood tests, sputum cultures, or CT scans are often needed.
Antibiotics won’t help. You need antifungals. Amphotericin B for severe cases, fluconazole or itraconazole for milder ones. Treatment can last months. Mortality is higher here-10-15% in immunocompromised patients-because the infection spreads beyond the lungs if not caught early.
How to Tell Them Apart
Here’s how the three types compare in real-world terms:
| Feature | Bacterial | Viral | Fungal |
|---|---|---|---|
| Onset | Sudden (hours) | Gradual (days) | Very slow (weeks) |
| Fever | High (102-105°F) | Mild to moderate (100-102°F) | Low-grade to moderate |
| Cough | Productive, colored mucus | Dry, worsening over time | Productive, sometimes bloody |
| Chest X-ray | One lobe, solid white area | Bilateral, hazy pattern | Nodules or cavities, often upper lobes |
| Primary Treatment | Antibiotics | Supportive care, antivirals if applicable | Antifungals |
| High-Risk Groups | Children, elderly, smokers | Infants, elderly, pregnant women | Immunocompromised, outdoor workers |
The biggest mistake? Giving antibiotics for viral pneumonia. The CDC reports that 30% of outpatient antibiotic prescriptions are unnecessary-and most of those are for viral infections. This doesn’t help the patient. It just fuels drug-resistant superbugs. That’s why doctors are turning to faster tests. New PCR panels can check for 20+ pathogens in one sample, with 95% accuracy. Soon, we might have blood tests that tell if an infection is bacterial or viral before you even get a chest X-ray.

Prevention: What Actually Works
You can’t avoid all germs-but you can reduce your risk.
- For bacterial pneumonia: Get the pneumococcal vaccine. The 20-valent version (Prevnar 20) protects against the most common strains. It’s recommended for kids under 2 and adults 65+. Even if you’re healthy, it cuts your risk by 60-70%.
- For viral pneumonia: Get your flu shot every year. It reduces pneumonia risk by 40-60%. Stay up to date on your COVID-19 boosters too. They cut pneumonia risk by up to 90% in the months after vaccination.
- For fungal pneumonia: If you’re in a high-risk job or live in an endemic area, wear a mask when digging in soil, cleaning bird droppings, or working in dusty buildings. Avoid disturbing soil in dry, arid regions.
Smoking? It doubles your risk. Quitting is one of the best things you can do for your lungs-no matter your age.
When to Worry
Not every cough needs a doctor. But if you have:
- Fever above 102°F with chills
- Coughing up blood or thick green/yellow mucus
- Chest pain that gets worse with breathing
- Shortness of breath that doesn’t improve
- Blue lips or fingertips
- Confusion or dizziness (especially in older adults)
-get checked. Pneumonia can look like the flu, a cold, or even heartburn. But if it’s left unchecked, it can turn into sepsis, respiratory failure, or death.
Can you get pneumonia from the flu shot?
No. The flu shot contains inactivated virus or just parts of the virus-it can’t cause infection. Some people feel mild side effects like soreness or a low-grade fever, but that’s your immune system responding, not the flu. You can still catch other viruses or bacteria after the shot, but you won’t get pneumonia from the vaccine itself.
Is fungal pneumonia contagious?
No. Fungal pneumonia isn’t passed from person to person. You catch it by breathing in spores from the environment-like soil, bird droppings, or dust. You can’t give it to someone else. That’s why it’s rare and mostly affects people with weakened immune systems.
Why do some people get pneumonia more than once?
Repeated pneumonia often signals an underlying problem. Chronic lung disease like COPD, uncontrolled diabetes, smoking, or a weakened immune system makes you more vulnerable. If you’ve had pneumonia twice in a year or three times in five years, you should see a specialist. Tests can check for hidden conditions like aspiration, immune disorders, or structural lung issues.
Can antibiotics cure viral pneumonia?
No. Antibiotics only work against bacteria. Giving them for viral pneumonia doesn’t help the virus, doesn’t speed recovery, and increases your risk of side effects like diarrhea or yeast infections. Worse, it contributes to antibiotic resistance. If a doctor prescribes antibiotics for a suspected viral infection, ask why-there should be a clear reason, like a secondary bacterial infection.
Are children more at risk for bacterial pneumonia?
Yes. Children under 2 are especially vulnerable because their immune systems are still developing. Before vaccines, Streptococcus pneumoniae is a bacterium that was the leading cause of pneumonia in young children worldwide. killed thousands each year. Since routine vaccination started, hospitalizations for bacterial pneumonia in kids have dropped by over 70%. That’s one of the biggest public health wins of the last 20 years.
Knowing the difference between bacterial, viral, and fungal pneumonia isn’t about memorizing medical terms. It’s about understanding how your body fights infection-and how to protect yourself. Whether you’re a parent, a caregiver, or someone with a chronic condition, the right knowledge can mean the difference between a few days off work and a hospital stay. Stay informed. Stay vaccinated. And don’t ignore a cough that won’t go away.
Kunal Kaushik
February 3, 2026 AT 16:43Man, this post hit different 😍 I just had my first pneumonia last year and honestly? I thought it was just a stubborn cold. Turns out it was bacterial-my doc said I was lucky I came in when I did. That fever hit 104°F and I swear my lungs felt like they were full of glue. Thanks for breaking it down so clearly.
Caleb Sutton
February 5, 2026 AT 00:36Antibiotics are a scam. Big Pharma pushes them so you keep coming back. Viral pneumonia is just your body’s natural detox. Stop poisoning yourself with drugs.
Jamillah Rodriguez
February 6, 2026 AT 02:03Okay but like… why does everyone always say "get the vaccine" like it’s magic? I got my flu shot last year and still got sick. Like… what’s the point??
Susheel Sharma
February 6, 2026 AT 10:02The structural inadequacy of public health messaging is glaring. You present data with clinical precision, yet the average individual lacks the epistemic scaffolding to interpret it. The disconnect between scientific literacy and populist discourse is not merely educational-it’s existential.
Janice Williams
February 7, 2026 AT 05:06You say "fungal pneumonia is rare in healthy people," but have you considered that this is precisely the narrative the CDC uses to downplay environmental hazards? The real issue is industrial soil contamination and corporate negligence. This isn't "nature"-it's systemic poisoning.
Roshan Gudhe
February 7, 2026 AT 07:20It’s wild how we treat lungs like they’re just air pipes. They’re living ecosystems. Bacterial pneumonia? That’s an invasion. Viral? That’s a civil war inside your alveoli. Fungal? That’s a slow colonization-like weeds taking over a neglected garden. We don’t just treat symptoms-we’re fighting wars in our own bodies. And we don’t even know half the soldiers.
Rachel Kipps
February 8, 2026 AT 11:14i read this whole thing and i think the part about antivirals for flu is super important. i had a friend who waited 5 days and then got really bad. like… time matters. just saying.
Katherine Urbahn
February 9, 2026 AT 22:58It is imperative to note that the assertion regarding the efficacy of pneumococcal vaccines is not universally substantiated by longitudinal cohort studies. Furthermore, the statistical reduction in hospitalizations may be confounded by concurrent improvements in ICU protocols and antimicrobial stewardship. One must remain vigilant against oversimplification of complex biomedical phenomena.
Joy Johnston
February 11, 2026 AT 12:37As a nurse who’s seen 12 cases of fungal pneumonia in immunocompromised patients, I can tell you: early diagnosis saves lives. The CT scans look like constellations of nodules-so easy to miss if you’re not looking. If you’re in a high-risk group and have a cough that won’t quit? Push for a fungal panel. Don’t wait for it to get "bad enough."
Shelby Price
February 11, 2026 AT 22:12Wait so… if I live in Ohio and I’m cleaning out my attic full of bird poop, am I basically playing Russian roulette with my lungs? 😅
Jesse Naidoo
February 12, 2026 AT 23:13I got pneumonia twice in two years. My doctor said it was "just bad luck." But I’ve been working construction since I was 18. I’m 32. I’m not lucky. I’m exposed. Nobody talks about how much dust we breathe in. This isn’t medical-it’s occupational.
Keith Harris
February 13, 2026 AT 23:23You call fungal pneumonia "rare"? That’s what they want you to think. The real numbers are buried under bureaucratic reporting. And why is it only "endemic" in certain areas? Because the government doesn’t want you to know how much of the soil is contaminated with spores from industrial farms and waste facilities. This is a cover-up.
Mandy Vodak-Marotta
February 15, 2026 AT 05:50I’m a 34-year-old mom of three and I just want to say-this was the most useful thing I’ve read in months. I used to think pneumonia was just "a bad cold you can’t shake." Now I know why my youngest kept coughing after the flu last winter. I got him the pneumococcal shot right away. Also, I finally threw out that dusty vacuum cleaner I’d been dragging around since 2018. Who knew? Clean air matters. I’m gonna print this out and put it on the fridge.
Nathan King
February 16, 2026 AT 05:37The epistemological framework underpinning this exposition is commendable. However, one must interrogate the underlying ontological assumption that pathogen taxonomy is sufficient to dictate clinical intervention. The reductionist model of categorizing pneumonia by etiology may obscure the emergent systemic dysregulation that characterizes all severe respiratory infections.
Harriot Rockey
February 17, 2026 AT 01:59This is why I love learning. I didn’t even know fungal pneumonia existed until now. I’m going to tell my uncle who works on the farm. He’s always brushing off his cough. And hey-I’m getting my flu shot this week. No excuses anymore. Thank you for writing this like you actually care. 🌱