When your pancreas swells up, it doesn’t just hurt-it can change your life. Pancreatitis isn’t just a bad stomach ache. It’s when your own digestive enzymes start eating away at your pancreas instead of breaking down food in your intestines. This isn’t rare. In the U.S. alone, over 275,000 people are hospitalized for acute pancreatitis every year. And for many, it doesn’t go away after a few days. It becomes chronic-lasting for years, slowly destroying your ability to digest food, regulate blood sugar, and even feel normal again.
What’s the Difference Between Acute and Chronic Pancreatitis?
Acute pancreatitis hits like a storm. One moment you’re fine; the next, you’re doubled over with sharp pain in your upper belly that shoots straight through to your back. Nausea, vomiting, fever-everything comes at once. This usually starts after drinking too much alcohol, having gallstones, or sometimes for no clear reason at all. The good news? About 80% of these cases clear up within a week with rest, fluids, and careful monitoring. Your pancreas can heal itself-if it hasn’t been damaged too badly. Chronic pancreatitis is different. It’s not a sudden event. It’s a slow burn. Over months or years, repeated inflammation turns healthy pancreatic tissue into scar tissue. Your pancreas stops working the way it should. You might still have pain, but it often gets less intense over time. That doesn’t mean you’re getting better. It means your pancreas is running out of cells to hurt. What’s left? Fatigue, weight loss, greasy floating stools (called steatorrhea), and eventually, diabetes. The numbers tell the story. While acute pancreatitis has a 5% overall death rate, severe cases can kill up to 30% of patients. Chronic pancreatitis doesn’t kill as quickly, but it’s relentless. Only 45% of people with chronic pancreatitis are alive 20 years after diagnosis. And 90% of them will lose their ability to digest food properly.How Doctors Diagnose Each Type
For acute pancreatitis, doctors look for three things: severe belly pain, blood tests showing lipase or amylase levels three times higher than normal, and imaging like a CT scan showing a swollen, inflamed pancreas. If two of these are present, it’s pancreatitis. The Revised Atlanta Classification, updated in 2012, now separates cases into mild, moderately severe, and severe-based on whether your organs (like your lungs or kidneys) start failing and for how long. Chronic pancreatitis is trickier. Blood tests often look normal, even when the pancreas is failing. The real clues come from imaging. A CT scan might show calcium deposits inside the pancreas-like tiny stones. An MRI can reveal ducts that are stretched, blocked, or broken. The M-ANNHEIM system breaks chronic pancreatitis into six stages, from early pain without damage to full organ failure. By the time most people get diagnosed, they’re already in the middle or late stages. And here’s something surprising: up to 30% of acute cases have no known cause. These are called idiopathic. For chronic cases, 70-80% are linked to long-term alcohol use. But genetics matter too. Mutations in genes like PRSS1 or SPINK1 can make someone prone to pancreatitis even if they never drink.Nutrition: The Forgotten Treatment
Most people think of pancreatitis as something you treat with painkillers and IV fluids. But nutrition? That’s where real recovery happens-and where most patients fall through the cracks. During an acute flare-up, your gut shuts down. You can’t eat. That’s normal. But here’s the key: you need to start feeding your body again within 24 to 48 hours. Not with fancy soups or broths. With enteral nutrition-liquid formula pushed directly into your small intestine through a tube. Studies show this cuts infection risk by 30% compared to feeding through a vein (parenteral nutrition). Your gut needs fuel to heal, even if you’re not hungry. Once you’re stable, you need protein. Around 1 to 1.5 grams per kilogram of body weight each day. That’s about 70-100 grams for most adults. Too little, and you lose muscle. Too much, and your pancreas struggles to process it.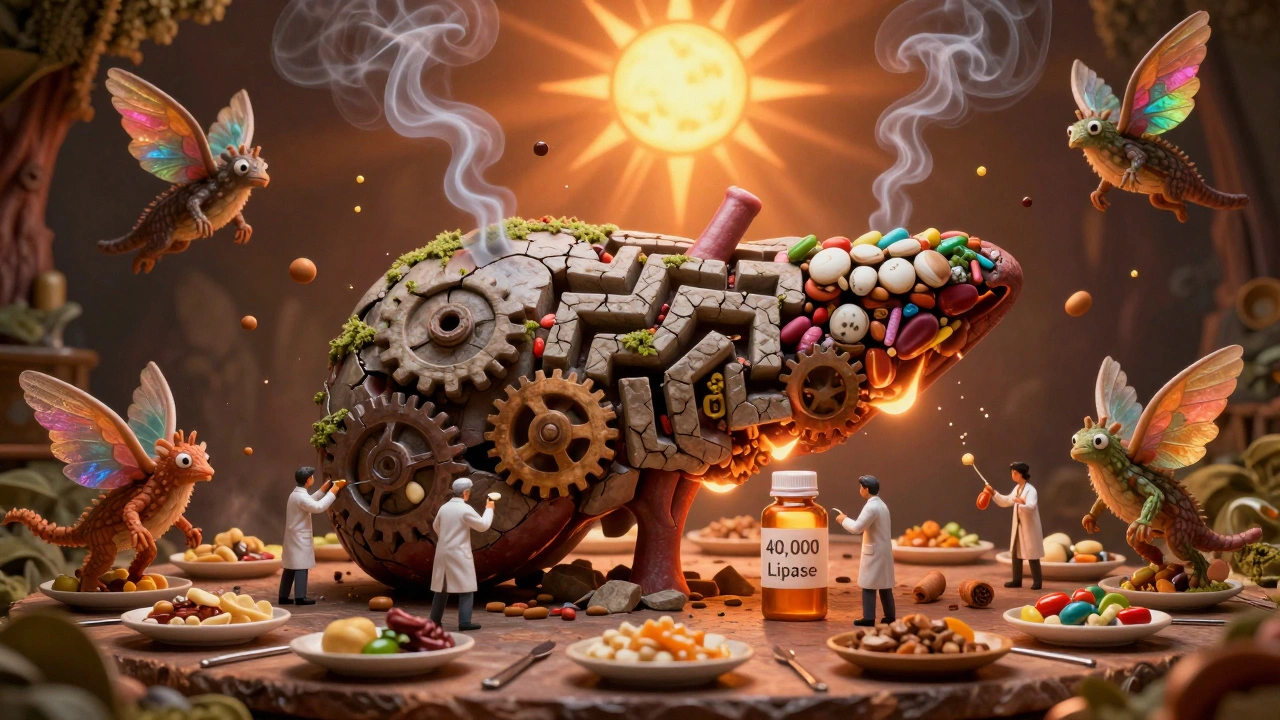
Chronic Pancreatitis and the Battle for Calories
If you have chronic pancreatitis, eating feels like a gamble. Every bite could trigger pain, bloating, or diarrhea. That’s why 42% of patients lose more than 10% of their body weight-not because they’re trying to diet, but because they’re scared to eat. The solution isn’t to eat less. It’s to eat smarter. First, pancreatic enzyme replacement therapy (PERT) is non-negotiable. You need enzymes to break down fat, protein, and carbs. Dosing matters. For meals, you need 40,000 to 90,000 lipase units. For snacks, 25,000. If you’re still having greasy stools, you’re underdosed. A 72-hour fecal fat test can tell you if your enzymes are working. Second, switch to medium-chain triglycerides (MCTs). These are special fats that don’t need pancreatic enzymes to be absorbed. Found in coconut oil and some medical formulas, MCTs give you calories without triggering steatorrhea. Many patients report fewer bathroom trips and better energy after switching. Third, eat small, frequent meals. Six to eight times a day. Large meals overwhelm your pancreas. Smaller ones let your body keep up. And yes-you still need fat. But keep it to 40-50 grams a day. Not zero. Fat isn’t your enemy. Lack of nutrients is.Deficiencies You Can’t Ignore
Your pancreas doesn’t just make enzymes. It helps your body absorb vitamins. When it fails, you get deficient-in ways you won’t feel until it’s too late. A 2023 study found that 85% of chronic pancreatitis patients had low vitamin D. 40% were low in B12. 25% lacked vitamin A. These aren’t just numbers. Low vitamin D means weak bones and more pain. Low B12 causes nerve damage and fatigue. Low vitamin A affects your vision and immune system. You need supplements. Not just a daily multivitamin. Targeted doses: 1,000-2,000 IU of vitamin D daily, 1,000 mcg of B12 (often as a sublingual tablet), and vitamin A in its pre-formed form (retinol), not beta-carotene. And if you’ve developed diabetes from pancreatitis? That’s called pancreatogenic diabetes. It’s different from type 1 or type 2. Your blood sugar swings wildly because your pancreas can’t release insulin smoothly. That’s why the FDA approved the Dexcom G7 continuous glucose monitor specifically for these patients in January 2024. It’s not a luxury-it’s a lifeline.

Jane Quitain
December 7, 2025 AT 10:30i had acute pancreatitis last year and honestly? the hardest part wasn't the pain-it was the guilt. like, i knew i shouldn't drink, but i thought 'just one beer' wouldn't hurt. yeah. it did. now i'm learning to eat again with enzymes and MCT oil. still messy, but better.
also, i typoed 'enzymes' as 'enzymes' like 3 times in my notes. sorry. my fingers have trauma.
David Brooks
December 8, 2025 AT 00:52OMG THIS POST IS A LIFESAVER 🙏
i thought i was just 'lazy' or 'bad at eating'-turns out i was just starving my pancreas while it was trying to scream for help.
started taking PERT and switched to coconut oil in my smoothies. my poop went from 'ocean' to 'normal' in 3 days. i’m crying. not because i’m sad-because i finally feel like i’m not broken.
if you’re reading this and you’re scared to eat? please try this. your body will thank you.
Olivia Hand
December 9, 2025 AT 05:32The narrative around pancreatitis is dangerously reductive. Most clinicians treat it like a 'lifestyle failure' when genetics and idiopathic cases account for nearly a third of acute presentations. The fact that 70-80% of chronic cases are alcohol-linked is statistically significant-but it’s weaponized to shame patients who never touched a drop.
And let’s talk about the vitamin deficiencies. Vitamin D isn’t just 'bone health'-it’s immunomodulatory. Low levels correlate with higher inflammatory cytokines in pancreatic tissue. That’s not anecdotal-it’s in the 2023 Gut paper. Yet primary care docs still hand out multivitamins like candy and call it a day.
Also, MCTs? Brilliant. But they’re not magic. They still require bile salts for micelle formation. If you’ve had cholecystectomy, you’ll need supplemental bile acids too. No one tells you that.
Desmond Khoo
December 11, 2025 AT 00:29bro i was in the hospital for 10 days with acute pancreatitis and the nurse gave me a pamphlet that said 'avoid fatty foods' and that was it. no enzymes. no vitamins. no MCTs. just 'go eat salad and pray'.
now i take 60k lipase units with every meal and i swear i’ve gained 8 lbs. not from junk food-from actual energy.
also, i bought a glucose monitor and it’s like having a personal body detective. 🤖💡
if you’re reading this and you’re scared to eat? just start with 1 tsp of coconut oil. your gut will whisper 'thank you'.
Louis Llaine
December 12, 2025 AT 03:23Wow. A whole 2000-word essay on how to not die from eating. Groundbreaking.
Next up: 'How to Survive Breathing: A Guide to Not Suffocating in Air'.
Also, 'pancreatic enzyme replacement therapy'-because nothing says 'modern medicine' like shoving powdered pig guts into your smoothie.
And yes, I know this is serious. But the performative wellness tone? The 'you can recover!' pep talk? It’s exhausting. Some of us aren’t here to be inspirational posters.
Some of us are just trying to not vomit while our organs turn to concrete.
Sam Mathew Cheriyan
December 13, 2025 AT 20:17lol so pancreatitis is caused by alcohol and smoking? nahhh.
you know what really causes it? the government. they put fluoride in the water to kill your pancreas so you’ll need more insulin and become dependent on pharma.
also, MCT oil? that’s just coconut oil. coconut oil is from the secret society that controls the world. they want you to think it’s healthy so you’ll stop questioning the vaccines.
and the glucose monitor? that’s a tracking chip. i checked the firmware.
just drink water. and pray. and don’t trust doctors. they work for the pancreas cartel.
Nancy Carlsen
December 15, 2025 AT 11:35to anyone reading this who feels alone: you’re not.
i’m a nurse in Texas. i’ve seen patients lose 50 lbs, cry because they can’t hug their grandkids without pain, and still show up every day to take their enzymes like a soldier.
you’re not broken. you’re adapting.
and yes, it’s unfair that specialists are 4 months away. but you can still build your own care team-find a dietitian, join a support group, read the studies. you’re smarter than the system thinks you are.
you’ve got this. and i’m rooting for you. 🌻💛
Ted Rosenwasser
December 17, 2025 AT 03:00How quaint. You all treat this like a dietary lifestyle tweak. The truth? Pancreatic exocrine insufficiency is a metabolic catastrophe. You’re not 'eating smarter'-you’re performing biochemical triage with a spoon.
And let’s not romanticize MCTs. They’re absorbed via the portal vein, bypassing the lymphatic system, which alters lipid signaling pathways. This isn’t 'health hack' territory-it’s pathophysiological band-aiding.
Also, the Dexcom G7? FDA-approved for 'pancreatogenic diabetes'? That’s a marketing term, not a clinical one. The correct term is Type 3c diabetes. If you can’t even get the taxonomy right, why should I trust your enzyme dosing advice?
Ashley Farmer
December 18, 2025 AT 14:34i read this while sitting in the waiting room before my third endoscopy this year.
thank you for not saying 'just quit drinking' like everyone else. i’ve never drunk. i was 12 when it started.
the enzymes, the MCT oil, the vitamin D-i’ve been doing all of it. but no one ever talks about how lonely it is to carry this. to be the person who eats 6 times a day while everyone else has dinner.
you’re not just giving info. you’re giving permission to be tired. to be weird. to still be alive.
thank you.
Nicholas Heer
December 19, 2025 AT 09:55AMERICA IS DYING FROM PANCREATITIS BECAUSE THE GOVERNMENT BANNED FATS IN THE 90S AND FORCED US TO EAT CARBS. THAT’S WHY WE’RE ALL FAT AND OUR PANCREASES ARE MELTING.
THEY WANT YOU TO THINK IT’S ALCOHOL OR SMOKING-BUT IT’S THE FEDS. THEY CONTROL THE ENZYMES. THEY CONTROL THE OIL.
THEY EVEN MADE THE DEXCOM G7 TO TRACK YOUR BLOOD SUGAR SO THEY CAN SELL YOU INSULIN.
AND DON’T YOU DARE TELL ME MCT OIL IS NATURAL. COCONUT IS A CULTIVATED WEAPON.
TRUST NO ONE. EAT MEAT. NO CARBS. NO OIL. JUST STEAK. AND PRAY TO THE OLD GODS.
Sangram Lavte
December 20, 2025 AT 00:18i’m from India, and here, pancreatitis is often blamed on spicy food. but i’ve seen patients who never ate anything hot get it anyway.
the real issue? access. my cousin had chronic pancreatitis. couldn’t afford enzymes. had to use turmeric and ginger. it didn’t help much.
but we found a local pharmacy that sold generic lipase. 1/10th the price. now he eats. sleeps. smiles.
if you’re struggling with cost-ask your pharmacist. there’s always a cheaper way. just don’t give up.
Stacy here
December 21, 2025 AT 04:33we’ve been lied to. pancreatitis isn’t a disease-it’s a spiritual awakening. your pancreas is screaming because your soul is out of alignment. the enzymes? they’re just symbols. the real cure is fasting under a full moon while listening to Tibetan bowls.
the medical system wants you dependent on pills and monitors. but the truth? your body is a quantum organ. it heals when you stop trying to control it.
the MCT oil? it’s a placebo. the real magic is in surrender.
and the Dexcom? it’s not measuring glucose-it’s measuring your vibrational frequency. you’re either in sync… or you’re not.
ask yourself: who are you really feeding?
your pancreas? or your fear?