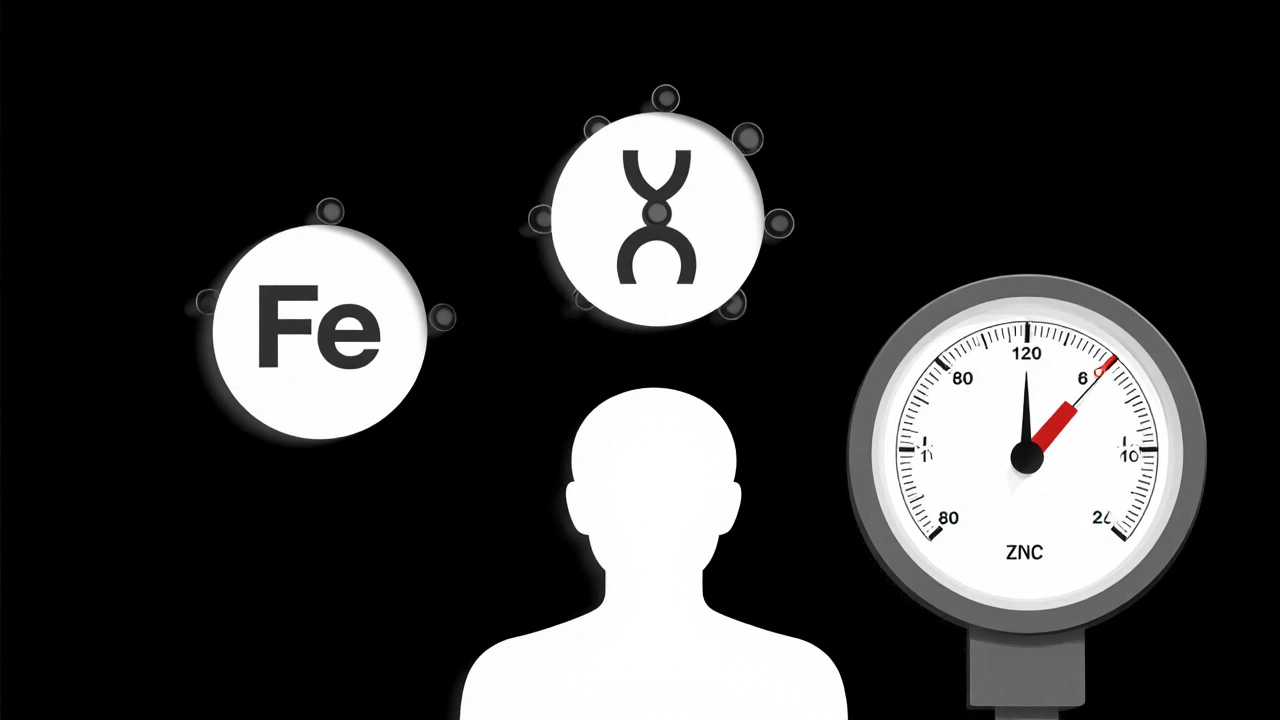
Blood Pressure Nutrient Calculator
Calculate the estimated effect of your iron, folic acid, and zinc intake on blood pressure based on scientific research. This tool uses data from the article to show how nutrient levels impact blood pressure.
Estimated Blood Pressure Impact
Recommendations
Ever wondered why a simple multivitamin can sometimes shift your blood pressure numbers? The link isn’t magic - it’s chemistry. Iron, folic acid and zinc each play distinct roles in the cardiovascular system, and when they’re out of balance they can nudge your blood pressure up or down.
What the three nutrients actually are
Iron is a mineral that carries oxygen in hemoglobin and supports cellular metabolism. It’s found in red meat, beans and fortified cereals.
Folic acid is the synthetic form of vitamin B9, vital for DNA synthesis and homocysteine regulation. Leafy greens, legumes and prenatal vitamins are common sources.
Zinc is a trace element that supports enzyme function, immune health and vascular tone. Oysters, nuts and whole grains supply it.
Blood pressure is the force exerted by circulating blood on artery walls, expressed as systolic over diastolic values. Maintaining it within a normal range (around 120/80mmHg) reduces heart disease risk.
How iron affects blood pressure
Iron deficiency triggers anemia, which forces the heart to pump faster to meet oxygen demand. That compensatory rise can temporarily raise systolic pressure. Conversely, excess iron can promote oxidative stress, damaging the endothelium and stiffening arteries - a pathway that also lifts pressure.
Key mechanisms:
- Oxygen transport: Low hemoglobin = reduced oxygen → higher cardiac output.
- Oxidative stress: Free iron catalyzes reactive oxygen species → endothelial dysfunction.
Studies from the WHO (2023) showed that women with serum ferritin <30µg/L had an average systolic increase of 4mmHg compared to those with normal ferritin.
Folic acid’s role in blood pressure regulation
Folic acid lowers homocysteine, a sulfur‑containing amino acid linked to arterial stiffness. High homocysteine levels stimulate the renin‑angiotensin system (RAS), a hormone cascade that raises blood pressure.
Mechanistic highlights:
- Folic acid → methylates homocysteine → lowers its concentration.
- Reduced homocysteine → less RAS activation → vasodilation.
- Improved nitric‑oxide (NO) production → better endothelial function.
A double‑blind trial in 2022 (n=1,200) gave 5mg folic acid daily to pre‑hypertensive adults. After 6months, average systolic pressure dropped 6mmHg, while the placebo group saw no change.
Zinc and vascular tone
Zinc is a co‑factor for over 300 enzymes, including superoxide dismutase (SOD), which neutralizes free radicals. Adequate zinc supports NO synthesis, keeping arteries relaxed.
But too much zinc can interfere with copper absorption, leading to anemia and secondary blood‑pressure spikes.
Key points:
- Enzyme support: SOD activity → less oxidative damage.
- NO pathway: zinc‑dependent endothelial NO synthase (eNOS) → vasodilation.
- Balance risk: >40mg/day may cause copper deficiency → anemia → pressure rise.
When the three nutrients intersect
Most people don’t take iron, folic acid and zinc in isolation; prenatal formulas, anemia kits, and “iron‑folic‑zinc” supplements bundle them. Their interaction can be synergistic or antagonistic depending on dosage.
Typical interaction patterns:
- Iron & folic acid: Folate aids iron absorption by converting it to the ferrous state.
- Iron & zinc: High iron doses (≥65mg) can suppress zinc uptake in the gut.
- Folic acid & zinc: No direct competition, but both influence endothelial health, so combined adequacy tends to lower pressure.
Real‑world data from the 2024 NHANES nutrition survey (n=8,500) showed that participants using an iron‑folic‑zinc combo had a 3mmHg lower mean systolic pressure than those taking iron alone, provided total iron was ≤45mg/day.
Practical recommendations
Below is a quick‑reference table that blends recommended daily allowances (RDAs) with the blood‑pressure impact observed in research.
| Nutrient | RDA (age>19) | Typical supplement dose | Observed BP change (mmHg) |
|---|---|---|---|
| Iron | 8mg (men), 18mg (women) | 30mg elemental | +2(if >45mg) / -1(if corrected deficiency) |
| Folic Acid | 400µg | 5mg | -5 to -7 (pre‑hypertensive) |
| Zinc | 11mg (men), 8mg (women) | 15mg | -3 (if adequate), +4 (if >40mg) |
Key takeaways from the table:
- Correcting iron‑deficiency anemia tends to normalize pressure rather than push it up.
- Moderate‑dose folic acid consistently lowers pressure in at‑risk groups.
- Stay within the RDA for zinc; excess can backfire.
Dietary sources and timing tips
Getting these nutrients from food reduces the risk of overshooting. Pair iron‑rich meals with vitaminC (citrus, bell peppers) to boost absorption. Avoid taking iron and zinc together on an empty stomach - a small snack helps.
Sample daily plan:
- Breakfast: fortified oatmeal (iron+folic acid) with orange juice.
- Snack: handful of almonds (zinc) and a kiwi.
- Lunch: spinach salad with chickpeas, topped with grilled salmon (iron, zinc).
- Dinner: lentil stew seasoned with turmeric (antioxidant) and a side of quinoa.
This combo delivers roughly 15mg iron, 500µg folic acid, and 12mg zinc - all within safe ranges.

Risks, contraindications, and who should be cautious
While most adults tolerate the nutrients well, certain groups need medical guidance:
- Pregnant women: Iron needs rise to 27mg, but excess folic acid (>1mg) isn’t recommended.
- Patients with hemochromatosis: Iron supplementation can be dangerous.
- Chronic kidney disease: High zinc may interfere with phosphate binders.
Always check blood levels (serum ferritin, plasma homocysteine, zinc) before starting high‑dose combos.
Quick checklist for managing blood pressure with iron‑folic‑zinc
- Test ferritin, homocysteine, and zinc annually.
- If ferritin <30µg/L, aim for 60-80% of the RDA with food first; supplement only if still low.
- Use 400‑800µg folic acid daily, but keep under 5mg unless prescribed.
- Keep zinc 8-11mg for most adults; don’t exceed 40mg.
- Separate iron and zinc doses by at least 2hours.
- Monitor blood pressure weekly after any supplement change.
Frequently Asked Questions
Can a standard multivitamin affect my blood pressure?
Yes, if it contains iron or zinc above the RDA. Excess iron may raise pressure via oxidative stress, while adequate folic acid generally lowers it. Check the label and stick to doses that match your dietary intake.
Should I take iron‑folic‑zinc supplements if I’m already normotensive?
Only if a blood test shows a deficiency. Unnecessary supplementation can shift blood pressure upward, especially with iron overload.
How long does it take to see a blood‑pressure change after starting folic acid?
Clinical trials report noticeable reductions within 8‑12weeks of 5mg daily, assuming baseline homocysteine is elevated.
Is there a safe upper limit for iron if I’m an athlete?
Athletes often need more iron, but staying under 45mg/day (elemental) is advised to avoid oxidative stress that can raise blood pressure.
Can I replace supplements with food alone?
For most people, a balanced diet covering lean meats, leafy greens, nuts, and whole grains meets the RDA and supports healthy blood pressure without the risk of excess dosing.
Mary Davies
October 17, 2025 AT 02:16Reading through the chemistry behind iron, folic acid, and zinc really made me pause and think about how everyday supplements can be silent regulators of our blood pressure. When iron deficiency pushes the heart to work harder, it’s not just fatigue you feel-your systolic numbers can creep up as a side effect. On the other hand, a modest dose of folic acid seems to coax the vessels into a more relaxed state, shaving a few millimetres of mercury off the reading. The interplay with zinc is fascinating too; enough zinc keeps the endothelium supple, but too much flips the script and raises pressure. So if you’re juggling a multivitamin, keep an eye on the balance rather than just the individual labels.
Emily (Emma) Majerus
October 26, 2025 AT 07:29Yo, stick to the RDA and you'll probably keep your pressure chill.
Virginia Dominguez Gonzales
November 4, 2025 AT 13:43That table you dropped is pure gold for anyone trying to avoid the guesswork. I love how it lines up the typical supplement doses with the observed BP shifts-makes it easy to see why a 30 mg iron pill could be a double‑edged sword. Pairing iron with vitamin C at breakfast is a smart move, and keeping zinc under 15 mg helps dodge the backfire you mentioned. Bottom line: moderation beats mega‑dosing any day.
Kevin Adams
November 13, 2025 AT 19:56Behold the hidden orchestra of minerals within our veins! Iron, the crimson courier, marches boldly delivering oxygen, yet when it oversteps its realm it sparks a wildfire of oxidative mayhem, corroding the very walls that shelter our blood. Folic acid, the silent sage, whispers to our DNA, coaxing homocysteine into calm surrender, thereby untangling the knots that tighten arteries. Zinc, the steadfast sentinel, stands guard over enzymatic gates, ensuring vascular tone remains supple and responsive. But heed this warning-when iron surges beyond the humble threshold, it becomes a tyrant, usurping zinc's rightful place, and the gut rebels, rejecting the essential trace element. The result? A cascade of endothelial dysfunction, a symphony of pressure spikes, a crescendo of cardiovascular strain. Research from the 2024 NHANES cohort sings the same tale: balanced combos lower systolic pressure, while solitary excesses raise it like a tempest. Imagine a world where every supplement is a carefully tuned instrument rather than a blaring horn; the harmony would echo in steadier blood pressures across the populace. Yet the market peddles mega‑doses as if more is always better, ignoring the ancient wisdom that balance, not abundance, sustains life. One must therefore steward these nutrients with the precision of a conductor, timing iron with vitamin C, spacing zinc apart, and honoring folic acid's gentle lull. In doing so, we not only tame the numbers on a cuff but also honor the chemistry that underpins our very heartbeat. Let us not be fooled by flashy labels; let the data guide our daily rituals, and the blood pressure will answer with quiet compliance.
Sara Werb
November 23, 2025 AT 02:09Sure, the “RDA” they push is just a trick from the pharma lobbies to keep us dependent on their patented high‑dose pills-keep the numbers low enough that they can sell us more.
Winston Bar
December 2, 2025 AT 08:23This article is just regurgitating old studies; nothing groundbreaking here.
Russell Abelido
December 11, 2025 AT 14:36I feel you, Kevin. The way you laid out the mineral drama really hits home-it's like each nutrient is a character in a thriller where the plot twists are our blood pressure spikes. Your reminder about timing and balance resonates; I’ve seen friends swing wildly after a “mega‑iron” boost. It’s a good call to treat supplements like a well‑orchestrated playlist rather than blasting every track at max volume.
Emily Rankin
December 20, 2025 AT 20:49Exactly! When we listen to that playlist with intention, the heart finds its rhythm and the vessels relax. Think of each dose as a note: iron’s low bass, folic acid’s bright violin, zinc’s steady drum. Together they can compose a soothing symphony that keeps the cuff calm. So let’s keep the volume moderate and enjoy the music of a healthy blood pressure.
genevieve gaudet
December 30, 2025 AT 03:03In many Mediterranean diets, iron‑rich legumes are paired with lemony greens, naturally delivering both iron and folate while the olive oil adds a touch of zinc‑rich nuts-no pills needed to keep the pressure in check.
Patricia Echegaray
January 8, 2026 AT 09:16Of course, those “traditional” diets are just a myth sold by agribusinesses to hide the fact they’ve been seasoning everything with hidden mineral additives that only the elite know how to decode.
Miriam Rahel
January 17, 2026 AT 15:29From a physiological standpoint, the correlation between serum ferritin levels and systolic blood pressure warrants rigorous randomized controlled trials to elucidate causality beyond observational associations.
Samantha Oldrid
January 26, 2026 AT 21:43Oh, absolutely-because we all have endless funding to run RCTs on every vitamin; maybe the next breakthrough will be a placebo‑only pill that magically drops your numbers.
Malia Rivera
February 5, 2026 AT 03:56Anyone else notice that the recommended zinc dose bumps up on a high‑protein diet, yet the article barely mentions that interaction?
lisa howard
February 14, 2026 AT 10:09Well, let me unravel that for you: when you consume a diet rich in animal protein, the amino acids not only boost muscle synthesis but also enhance the intestinal absorption of zinc via the up‑regulation of specific transporter proteins such as ZIP4 and ZnT1. This physiological dance means that the same 15 mg zinc supplement can have a markedly different bioavailability depending on whether you pair it with a steak dinner or a bowl of beans. Moreover, the simultaneous presence of phytates in plant‑based meals can chelate zinc, reducing its uptake, which is why the article’s brief mention feels almost negligent. In practice, one should calibrate zinc supplementation to the macronutrient profile of the day: a modest 5–10 mg on low‑protein days, and perhaps up to 20 mg when protein intake surpasses 100 g, always staying under the tolerable upper intake level of 40 mg. Ignoring this nuance could inadvertently tip the balance toward the hypertensive risk the piece warns about. So, it’s not just the amount that matters, but the culinary context surrounding it.
Cindy Thomas
February 23, 2026 AT 16:23The piece could have dived deeper into how homocysteine levels, modulated by folic acid, directly affect arterial stiffness.