Prostate Symptom Checker
Symptom Assessment Tool
Based on CDC guidelines, this tool helps identify potential prostate complications from gonorrhea. If symptoms persist after 2 weeks, see a healthcare provider.
When it comes to men’s health, the connection between Gonorrhea and prostate health often goes unnoticed until problems arise. Understanding how this common STI can affect the prostate, what signs to watch for, and how to protect yourself is crucial for staying healthy and avoiding long‑term complications.
Key Takeaways
- Gonorrhea can spread to the prostate, leading to bacterial prostatitis.
- Symptoms often overlap with other urological issues, making diagnosis tricky.
- Prompt testing and the right antibiotic regimen cure most infections.
- Using condoms and regular STI screenings are the best preventive measures.
- Follow‑up care is essential to ensure the prostate fully recovers.
What Is Gonorrhea and Why It Matters for the Prostate
Gonorrhea is a bacterial sexually transmitted infection caused by Neisseria gonorrhoeae. It usually starts in the urethra, but if left untreated, the bacteria can travel upward through the urinary tract and reach the prostate gland.
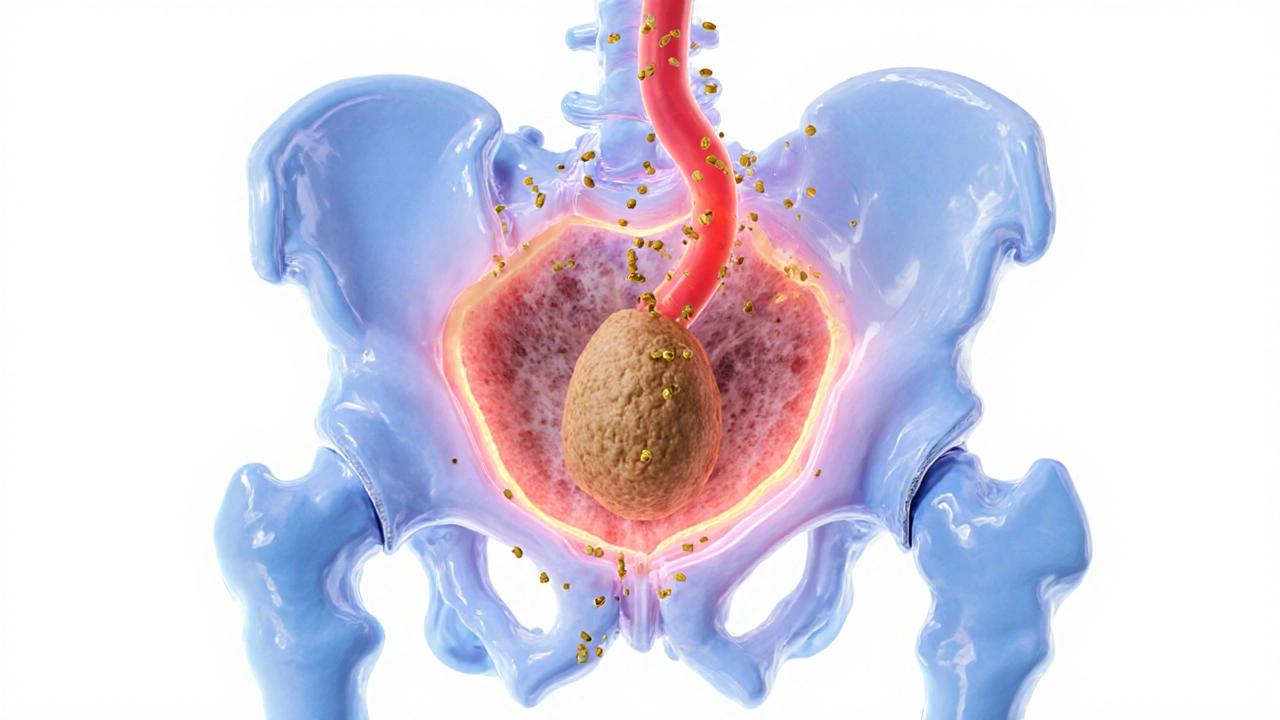
The prostate gland is a walnut‑sized organ that produces seminal fluid. When gonorrhea infects this gland, it triggers inflammation known as bacterial prostatitis. This condition can cause persistent pelvic pain, urinary issues, and, in severe cases, affect fertility.
How Gonorrhea Leads to Prostatitis
The pathway from a urethral infection to prostate inflammation typically follows these steps:
- The bacteria colonize the urethra, causing urethritis.
- Through the prostate’s ducts, the pathogen ascends into the prostate tissue.
- The immune response creates swelling, fluid buildup, and pain.
Studies from the Centers for Disease Control and Prevention (CDC) show that up to 15% of untreated male gonorrhea cases develop complications, with prostatitis being one of the most common.

Spotting the Signs: Symptoms Overlap and Red Flags
Both gonorrhea and prostatitis share symptoms such as burning during urination, frequent urge to pee, and discomfort in the perineum. However, prostate‑specific signs often include:
- Dull, aching pain in the lower back or hips.
- Difficulty starting or stopping urine flow.
- Painful ejaculation or blood in semen.
- Elevated PSA test levels, though not always present.
If any of these symptoms appear within two weeks of a suspected STI exposure, it’s time to seek medical evaluation.
Testing, Diagnosis, and Effective Treatment
Accurate diagnosis hinges on two main steps: confirming the presence of gonorrhea and assessing prostate involvement.
For gonorrhea, the CDC recommends nucleic acid amplification tests (NAAT) on urine samples or urethral swabs. These tests detect bacterial DNA with over 99% accuracy.
If prostatitis is suspected, doctors may order a digital rectal exam (DRE) plus a prostate secretion analysis. Culturing the fluid helps identify the exact strain and antibiotic sensitivity.
First‑line treatment for uncomplicated gonorrhea now includes a single intramuscular dose of ceftriaxone (500mg) combined with oral doxycycline for 7 days to cover possible co‑infection with chlamydia. For bacterial prostatitis, a longer course-typically 4‑6 weeks-of fluoroquinolones or trimethoprim‑sulfamethoxazole is prescribed, depending on susceptibility.
Completing the full antibiotic regimen is non‑negotiable; stopping early can lead to chronic infection and antibiotic resistance.
Prevention: Reducing the Risk of Prostate Involvement
Prevention strategies focus on both avoiding infection and protecting the prostate if exposure occurs.
- Consistently use latex or polyurethane condoms during vaginal, anal, and oral sex.
- Undergo regular STI screenings-at least once a year for sexually active men, more often with multiple partners.
- Limit the number of concurrent sexual partners and discuss STI status openly.
- Seek prompt treatment if any STI symptoms arise, even mild ones.
Vaccines currently do not exist for gonorrhea, but ongoing research aims to develop a protective immunization in the next few years.

Managing Long‑Term Prostate Health After an STI
Even after successful treatment, some men experience lingering prostate discomfort. Here’s a practical roadmap:
- Follow‑up testing: Repeat NAAT or culture 2-3 weeks post‑treatment to confirm eradication.
- Monitor PSA levels: Baseline PSA before infection and re‑check after 3 months to ensure no chronic inflammation.
- Adopt lifestyle habits: Stay hydrated, limit caffeine/alcohol, and incorporate regular pelvic floor exercises.
- Consider physiotherapy: Targeted massage or heat therapy can relieve residual muscle tension around the prostate.
- Seek specialist care: Urologists can provide additional diagnostics like transrectal ultrasound if symptoms persist.
Most men recover fully, but staying vigilant prevents chronic prostatitis, which can affect quality of life and sexual function.
Quick Reference Table: Gonorrhea vs. Bacterial Prostatitis
| Aspect | Gonorrhea (Urethral) | Bacterial Prostatitis |
|---|---|---|
| Primary site | Urethra | Prostate gland |
| Typical onset | Within days of exposure | 1-2 weeks after untreated gonorrhea |
| Common symptoms | Burning urination, discharge | Painful ejaculation, back pain, urinary hesitancy |
| Diagnostic test | NAAT urine or swab | DRE + prostate fluid culture |
| Treatment duration | Single dose + 7‑day doxycycline | 4-6 weeks of targeted antibiotics |
Frequently Asked Questions
Can gonorrhea cause permanent prostate damage?
If treated promptly, permanent damage is rare. Chronic infection or delayed treatment can lead to scarring, which may affect urinary flow and sexual function.
Is a PSA test useful for diagnosing prostatitis from gonorrhea?
PSA can be elevated during inflammation, but it’s not specific. It helps rule out prostate cancer when combined with other assessments.
Do I need to inform my partner if I was treated for gonorrhea‑related prostatitis?
Yes. Both partners should be tested and treated to prevent reinfection. Open communication reduces the spread of STIs.
Can condoms fully protect the prostate from gonorrhea?
When used correctly, condoms dramatically lower the risk of urethral infection, which in turn protects the prostate. They are not 100% foolproof but remain the best barrier method.
What lifestyle changes help recovery after prostatitis?
Stay well‑hydrated, avoid caffeine and alcohol, practice regular pelvic floor stretches, and maintain a balanced diet rich in antioxidants to support tissue healing.
Richard Phelan
October 12, 2025 AT 12:52Alright folks, let’s get real about gonorrhea and the prostate. This isn’t some mythic beast that appears out of nowhere; it’s a bacterial invader that can set up camp in your prostate if you ignore it. The CDC says untreated cases can spiral into chronic prostatitis, and that’s a nightmare for anyone who values a pain‑free life. So, the moment you notice burning urination or a strange discharge, book that doctor’s appointment-no excuses. And remember, condoms aren’t just for the birds; they’re the first line of defense for your prostate health too.
Suman Wagle
October 12, 2025 AT 13:59If you think the universe cares about your urethra, you’re in for a surprise-nothing in nature respects our laziness. Gonorrhea’s little ambition is simply to colonize the nearest warm tissue, and the prostate is just a conveniently quiet suburb. So, treat it like a philosophical lesson: ignorance isn’t bliss, it’s a prescription for chronic discomfort. Luckily, modern medicine offers a quick fix, if you’re willing to act before the irony becomes your reality.
Neil Sheppeck
October 12, 2025 AT 15:05Early testing is the simplest way to keep the prostate out of the drama.
Stephanie S
October 12, 2025 AT 16:12When it comes to sexual health, - especially regarding gonorrhea and its potential impact on the prostate - there are a few non‑negotiables, - use condoms, get screened regularly, and seek treatment promptly, - otherwise you risk a cascade of urological complications.
Bradley Fenton
October 12, 2025 AT 17:19Get tested, take the full antibiotic course, and stay hydrated; that’s the three‑step recipe for recovery.
Wayne Corlis
October 12, 2025 AT 18:25I have to say, watching through the minutiae of gonorrhea‑related prostatitis feels like watching a slow‑motion train wreck that you could have avoided if you’d simply looked at the timetable. First, the bacterium Neisseria gonorrhoeae is a master of opportunistic colonisation, slipping through the urethral gate with the stealth of a cat burglar. Once it reaches the prostate, the immune system throws a tantrum, causing inflammation that radiates down the pelvic floor like a bad Wi‑Fi signal. What’s truly maddening is how the symptoms masquerade as ordinary urinary irritation, lulling men into a false sense of normalcy. Doctors often have to play detective, ordering NAAT tests and sometimes a digital rectal exam just to confirm what the patient should have suspected earlier. The treatment protocol-single‑dose ceftriaxone plus a week of doxycycline-might sound simple, but compliance is the Achilles’ heel of the whole operation. Skipping the final days of antibiotics is essentially inviting the bacteria to set up a rebel outpost in the prostate, which can evolve into chronic prostatitis. Chronic cases, as you know, can lead to persistent pelvic pain, sexual dysfunction, and even anxiety about future fertility. And let’s not forget the psychosocial toll; men often feel embarrassed, leading them to hide symptoms and delay care even further. The best preventive measure, unsurprisingly, is consistent condom use, which, despite its reputation, remains the most effective barrier against urethral infection. Coupled with regular STI screening-ideally every six months for sexually active individuals-the risk drops dramatically. Lifestyle tweaks like staying well‑hydrated, limiting caffeine, and doing pelvic floor exercises can also mitigate lingering discomfort after treatment. If symptoms persist beyond the antibiotic window, a referral to a urologist for a transrectal ultrasound or prostate fluid culture is warranted. In my experience, patients who follow up diligently rarely suffer lasting damage, but the ones who ignore follow‑ups often become chronic pain sufferers. So the moral of the story is clear: early detection, full adherence to therapy, and proactive follow‑up are the holy trinity of prostate health in the context of gonorrhea. Ignore any of these steps, and you’re signing up for a future of unnecessary medical appointments and a dwindling quality of life.
Kartikeya Prasad
October 12, 2025 AT 19:32Seriously, guys, a quick NAAT test and a proper antibiotic regimen will zap that bug faster than you can say ‘oops’ 😅. Don’t let a little discharge turn into a lifelong saga, just be proactive!
HARI PRASATH PRASATH
October 12, 2025 AT 20:39If u dont get treatd on time, the prostatitc pain can be really harsh and fustigate your daily life.
Andrew Miller
October 12, 2025 AT 21:45I can’t help but feel a pang of dread when I think about the silent ache men endure after ignoring a simple infection. It’s a quiet tragedy that many just shrug off.
Brent Herr
October 12, 2025 AT 22:52We need to stop normalizing careless sex and expect everyone to act responsibly; using protection isn’t optional, it’s a moral duty to safeguard your prostate and your partner’s health.
Jill Brock
October 12, 2025 AT 23:59The sheer audacity of some people to think they can dodge STIs without condoms is cinematic-except the plot twists into chronic prostatitis, and trust me, that drama is not worth the tickets.
Andrew Stevenson
October 13, 2025 AT 01:05From a urological perspective, early antimicrobial intervention aligns with evidence‑based protocols to eradicate Neisseria gonorrhoeae before it infiltrates the prostatic ducts, thereby reducing inflammatory cytokine cascades and preserving ejaculatory function.
Kate Taylor
October 13, 2025 AT 02:12I understand how unsettling those symptoms can feel; the key is prompt NAAT testing, appropriate ceftriaxone administration, and diligent follow‑up to ensure the infection is fully cleared and the prostate returns to baseline.
Jamie Balish
October 13, 2025 AT 03:19Okay, let’s break this down step by step because I know a lot of folks get overwhelmed by medical jargon. First, the infection starts in the urethra-so you might notice discharge or burning. If untreated, the bacteria can travel upward and lodge in the prostate, causing prostatitis, which brings that deep pelvic ache we all dread. The good news? We have a clear treatment pathway: a single intramuscular ceftriaxone shot plus a week of doxycycline, which kills the bug and any lurking chlamydia. But you have to finish the whole course, no shortcuts. After antibiotics, schedule a follow‑up test, because lingering bacteria can cause chronic inflammation. Meanwhile, keep hydrated, avoid excessive caffeine, and maybe add some pelvic floor stretches to ease any residual soreness. And, of course, condom use is your best defense-don’t skip it! Stay proactive, stay healthy, and remember you’ve got a support system cheering you on.
Jeff Bellingham
October 13, 2025 AT 04:25The article presents accurate data; however, it could benefit from a more rigorous citation of the CDC statistics and a concise summary of treatment guidelines. Overall, the exposition is satisfactory.
Matthew Balbuena
October 13, 2025 AT 05:32Yo, just a heads up-make sure u get that test done quick an finish the meds whole, otherwise u might end up with chronic pain that’s a total buzzkill.
michael abrefa busia
October 13, 2025 AT 06:39Totally agree with the three‑step plan! 👍 Staying hydrated and finishing antibiotics are game‑changers. 💪
Dorothy Anne
October 13, 2025 AT 07:45Your health journey matters, and taking those simple steps can make a huge difference in long‑term wellbeing; keep up the good work!
Sharon Bruce
October 13, 2025 AT 08:52We're all proud to protect our bodies; ditch the reckless attitudes and wear protection-it's a patriotic act for personal health! 🇺🇸💥
True Bryant
October 13, 2025 AT 09:59Honestly, if you’re still debating condom efficacy after reading the CDC guidelines, you’re missing the point-consistent use cuts transmission risk by over 90%, period.