When someone starts taking an antipsychotic medication, the goal is clear: reduce hallucinations, calm delusions, and bring back some stability. But for many, the relief comes with a hidden cost-weight gain, high blood sugar, and rising cholesterol. These aren’t just inconveniences. They’re silent threats that can shorten lives. In fact, people with serious mental illness die 20 to 25 years earlier than the general population, and about 60% of those deaths are from heart disease and diabetes-conditions directly linked to the very drugs meant to help them.
Why Some Antipsychotics Are Harder on Your Body
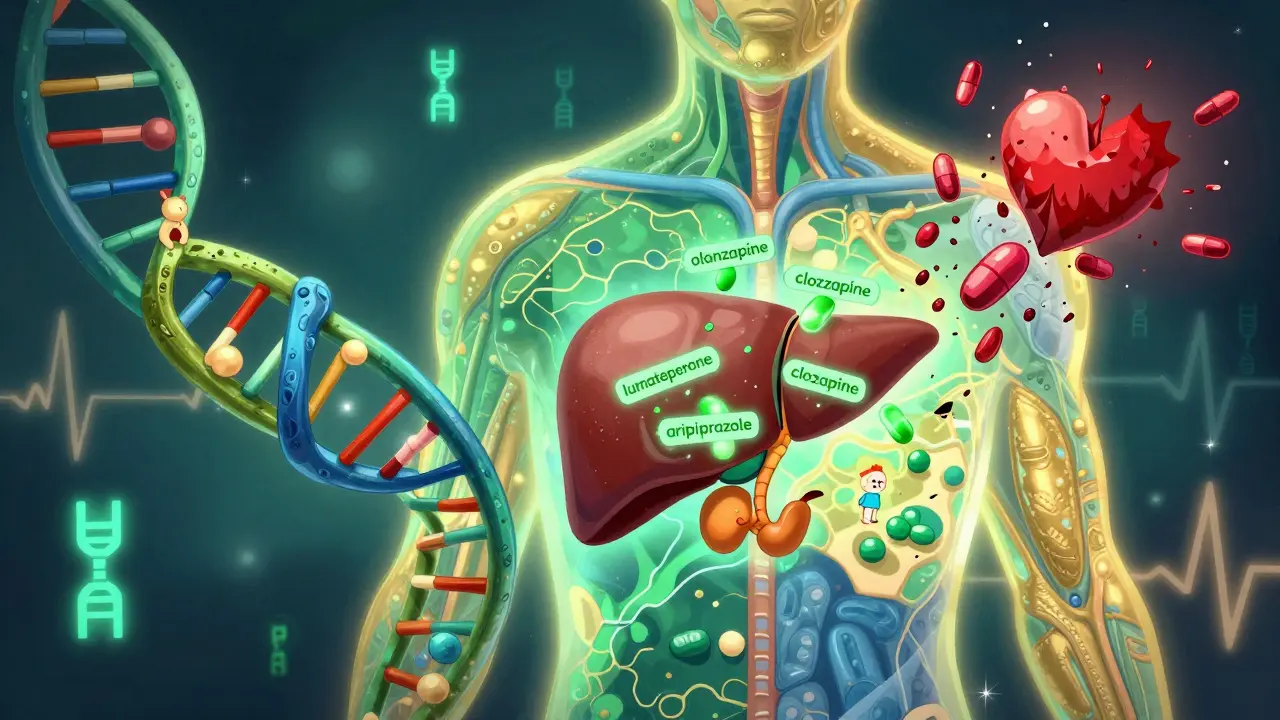
Not all antipsychotics are the same. The newer ones, called second-generation antipsychotics (SGAs), were designed to be safer for movement disorders like tremors and stiffness. But in the early 2000s, doctors started noticing a troubling pattern: patients on these drugs were gaining weight fast, developing type 2 diabetes, and showing abnormal cholesterol levels. The most concerning offenders? olanzapine and clozapine. In the CATIE study, patients on olanzapine gained an average of 2 pounds per month during the first 18 months. About 30% gained more than 7% of their body weight. That’s not just a few extra pounds-it’s a major health risk.Compare that to aripiprazole, ziprasidone, or lurasidone. These drugs have much lower metabolic risk. Only about 5% of people on aripiprazole gain significant weight. The difference isn’t random. It’s tied to how these drugs bind to brain receptors. Strong blocking of histamine H1 and serotonin 5-HT2C receptors leads to increased appetite and disrupted insulin control. That’s why clozapine and olanzapine-both heavy hitters at these receptors-are the worst offenders.
What Exactly Happens in Your Body?
It’s not just about eating more. Antipsychotics mess with your metabolism on a cellular level. They interfere with how your body processes sugar and fat, even before you gain weight. Some patients on olanzapine show high blood sugar and insulin resistance without any noticeable weight gain. Others develop low HDL (the "good" cholesterol) and high triglycerides, which together create a perfect storm for heart disease.Up to 68% of people on SGAs meet the criteria for metabolic syndrome-the cluster of conditions that raise your risk of heart attack, stroke, and diabetes. That’s compared to just 3.3% to 26% in people not taking these drugs. The numbers don’t lie: patients on SGAs are three times more likely to develop severe weight gain, type 2 diabetes, or cardiovascular disease than those not taking them.
The Monitoring Checklist: What Doctors Should Be Checking
There’s no excuse for not catching these problems early. Guidelines from the American Psychiatric Association and the American Diabetes Association are clear: before starting any antipsychotic, you need a full metabolic baseline. That means:- Weight and BMI
- Waist circumference (central obesity is a key marker)
- Blood pressure
- Fasting blood glucose
- Lipid panel (triglycerides, HDL, LDL)
After starting the medication, check again at 4 weeks, 8 weeks, and 12 weeks. Then, at least once a year-every year-for the rest of your life. Yet, a 2022 survey found only 38% of U.S. psychiatrists follow these guidelines consistently. Many patients never get their blood sugar checked. Some don’t even have their weight tracked.
Why? Time constraints, fragmented care, and the belief that "it won’t happen to me." But the data shows otherwise. In one UK study, 42% of patients said they were never monitored for metabolic side effects. That’s not negligence-it’s systemic failure.

What to Do If You’re Gaining Weight or Your Numbers Are Rising
If you’ve gained more than 5% of your body weight since starting your medication, it’s time to talk to your doctor. That’s the trigger point for lifestyle changes: better nutrition, more movement, and maybe a referral to a dietitian. If you’ve gained 7% or more, your doctor should seriously consider switching you to a lower-risk antipsychotic. Yes, that might mean your psychosis symptoms could flare up-but the trade-off might be worth it. Many patients report feeling more like themselves again after switching from olanzapine to aripiprazole, even if the antipsychotic effect is slightly less strong.Some patients choose to stick with high-risk meds like clozapine because it’s the only thing that controls their hallucinations. That’s valid. But even then, monitoring is non-negotiable. One patient on Reddit shared: "I gained 45 pounds on olanzapine. I had to switch-even though it wasn’t as good for my voices-because I was prediabetic and my knees were killing me."
New Options Are Coming-And They’re Better
The good news? The field is changing. In 2023, the FDA approved lumateperone (Caplyta), a new antipsychotic with a metabolic profile that’s dramatically better. In clinical trials, only 3.5% of users gained weight, compared to 23.7% on olanzapine. It’s not a miracle drug, but it’s a sign that pharmaceutical companies are finally listening.The National Institute of Mental Health is also funding a $12.5 million study to find genetic markers that predict who’s likely to gain weight or develop diabetes on antipsychotics. By 2025, we might be able to test a patient’s DNA before prescribing and pick the safest drug from the start. That’s the future-and it’s closer than you think.
Why This Matters Beyond the Numbers
This isn’t just about lab results. It’s about dignity, mobility, and quality of life. One woman in a UK mental health forum said: "I stopped taking my medication because I gained 30kg in a year and developed prediabetes. My psychiatrist didn’t even check my blood sugar." She wasn’t being non-compliant-she was surviving.Patients with serious mental illness already face stigma, isolation, and discrimination. Adding weight gain, diabetes, and heart disease on top of that is cruel. And it’s preventable. Integrated care models-where psychiatrists work with primary care providers to track weight, glucose, and blood pressure in the same visit-are working. Kaiser Permanente cut metabolic complications by 25% after implementing routine monitoring. It’s not rocket science. It’s basic care.
What You Can Do Right Now
If you’re on an antipsychotic, here’s what to do:- Ask for your baseline metabolic tests-right now, before you start or if you’ve been on it for a while.
- Keep a log of your weight and waist size every month.
- Request your last lipid panel and fasting glucose results. If you don’t know them, you’re not being monitored.
- Don’t accept "it’s just weight gain" as normal. It’s a medical red flag.
- Ask about switching to a lower-risk antipsychotic if your numbers are rising.
You deserve to be stable mentally-and physically. You don’t have to choose between sanity and health. Better options exist. Better care is possible. It just needs to happen.
Which antipsychotics have the lowest metabolic risk?
Aripiprazole, ziprasidone, and lurasidone have the lowest risk of weight gain, high blood sugar, and bad cholesterol. Lurasidone and aripiprazole are often preferred when metabolic health is a concern. Lumateperone (Caplyta), approved in 2023, is the newest option with a very favorable profile-only 3.5% of users gained weight in trials.
How often should metabolic tests be done?
Baseline tests (weight, waist, blood pressure, fasting glucose, lipids) must be done before starting any antipsychotic. Then repeat at 4, 8, and 12 weeks. After that, at least once a year. If you’re on a high-risk drug like olanzapine or clozapine, or if you’ve gained weight, testing every 3-6 months is recommended.
Can antipsychotic-induced weight gain be reversed?
Yes, but it’s harder than preventing it. Switching to a lower-risk antipsychotic often leads to gradual weight loss. Adding lifestyle interventions-like structured diet plans, regular exercise, and sometimes medications like metformin-can help. One study showed combining these approaches reduced weight gain by 50% in patients on antipsychotics.
Why don’t more doctors monitor metabolic health?
Many psychiatrists are overwhelmed, lack time, or work in systems where primary care and mental health aren’t connected. Some assume patients will see their GP-but many don’t. Others mistakenly believe metabolic side effects are inevitable. The truth? Monitoring is simple, cheap, and life-saving. The guidelines have existed since 2004-and yet, only 38% of U.S. psychiatrists follow them.
Is it safe to stop antipsychotics because of weight gain?
Never stop abruptly. Stopping suddenly can cause psychosis to return violently or trigger withdrawal symptoms. Instead, talk to your doctor about switching to a lower-risk medication. Many patients successfully transition from olanzapine to aripiprazole or lurasidone with good symptom control and improved metabolic health.
Are there any new drugs coming that are safer?
Yes. Lumateperone (Caplyta), approved in 2023, has significantly lower metabolic risk than older antipsychotics. Research is also underway to identify genetic markers that predict who will gain weight on certain drugs. By 2025, we may be able to match patients with the safest antipsychotic based on their DNA-making side effects preventable before they start.

Christina Bischof
December 16, 2025 AT 21:39Been on olanzapine for 3 years. Gained 50 lbs. My doc never checked my glucose until I passed out at work. Now I’m on aripiprazole and I feel like a human again. No more knee pain. No more prediabetes. Just me.
Nupur Vimal
December 18, 2025 AT 09:29Y’all are acting like this is news. I’ve been telling my shrink for years that these meds turn you into a blob. He just says ‘it’s the price of stability’ like I’m supposed to be okay with becoming a walking metabolic disaster. Wake up. This isn’t side effect-it’s malpractice.
Michelle M
December 19, 2025 AT 10:29It’s not just about the drugs. It’s about how we treat people with mental illness. We give them life-saving meds but then act like their bodies are someone else’s problem. You wouldn’t let someone with cancer go unmonitored for cholesterol-why are we doing this to people with schizophrenia? We’re not just failing them. We’re dehumanizing them.
Stability shouldn’t cost your dignity. You deserve to live-not just exist.
And yes, switching meds is scary. But staying on olanzapine because ‘it works’ is like keeping a broken leg in a cast because ‘it stops the bleeding.’
There’s a better way. We just have to choose it.
I’ve seen people lose 30 pounds after switching. I’ve seen them walk again. I’ve seen them laugh without guilt.
This isn’t medical advice. It’s a plea.
Ask for your labs. Push back. Demand better.
You’re not being dramatic. You’re being alive.
Lisa Davies
December 19, 2025 AT 17:25Just switched from clozapine to lumateperone last month 😊 I lost 8 lbs in 6 weeks and my triglycerides dropped like a rock. My psychiatrist actually asked me how I was feeling about my body-like, actually asked. I cried. It’s the first time anyone cared.
Also-metformin helped a TON. Not a cure, but a lifeline. 💪
Raj Kumar
December 21, 2025 AT 17:01As someone from India, this hits hard. We don’t have access to regular lipid panels or dietitians in most public hospitals. My cousin’s on olanzapine and his BMI is 38. No one’s checking. No one’s even asking. We need systemic change-not just individual hacks.
Also, aripiprazole is way underused here. Docs think it’s ‘weaker’ so they avoid it. But weaker isn’t worse if it keeps you alive.
And yes, I’ve seen people die from diabetes because they were too ashamed to go to the clinic after gaining weight. Shame kills faster than psychosis.
Cassie Henriques
December 22, 2025 AT 17:00Metabolic syndrome criteria are based on Caucasian populations. Are we even validating these thresholds for South Asian, African, or Indigenous patients? HbA1c thresholds, waist circumference cutoffs-they’re all skewed. We’re misdiagnosing or missing risk in marginalized groups because the data was never inclusive.
And don’t get me started on how insurance denies metformin for ‘off-label’ use in antipsychotic-induced insulin resistance. It’s insane.
PS: Lumateperone’s 3.5% weight gain? That’s in a trial with strict diet/exercise controls. Real world? Probably higher. Still better than olanzapine tho 😅
Jake Sinatra
December 23, 2025 AT 02:28Let me be clear: this is not a failure of psychiatry. This is a failure of healthcare infrastructure. Psychiatrists are not primary care providers. We cannot be expected to track waistlines, glucose, and lipids on top of managing psychosis, suicidal ideation, and medication adherence. The system is broken-not the clinicians.
Until we integrate mental health into primary care, we’re putting the burden on the wrong people. And yes, patients should advocate for themselves-but they shouldn’t have to be their own case managers.
Stop blaming the doctors. Fix the system.
RONALD Randolph
December 24, 2025 AT 17:22Oh wow. Another liberal guilt-trip about weight gain. Next you’ll tell me we should give everyone a free kale smoothie and a therapist. Get real. These drugs save lives. People who can’t handle side effects shouldn’t be on them in the first place. You think we’re gonna let people with violent psychosis off their meds because they got chubby? That’s not medicine-that’s surrender.
And if you’re so worried about your health, why not just stop taking them? Oh wait-you’d go back to screaming at the walls. There’s your answer.
Benjamin Glover
December 25, 2025 AT 13:22Utterly predictable. American medical system at its finest: overprescribe, undermonitor, underfund, overblame. We’ve known this since 2004. The fact that 62% of psychiatrists still ignore guidelines isn’t ignorance-it’s institutional cowardice.
Meanwhile, in the UK, we have mandatory metabolic monitoring embedded in NHS protocols. It’s not rocket science. It’s basic duty of care.
And yes, switching to aripiprazole is often feasible. But only if your psychiatrist has the time, the training, and the bloody courage to do it.
Stop pretending this is about patient choice. It’s about systemic neglect.